From a risk/benefit perspective, water fluoridation is an unacceptably risky practice — a fact that is evident even if teeth are the only tissue in the body that one considers.
Modern research shows that fluoride ingestion (from water alone, or all sources combined) is far more likely to cause teeth to develop fluorosis than it is to prevent a cavity. As demonstrated below, both fluoridated water and total daily fluoride intake have weak relationships with tooth decay which are very difficult to detect in modern populations. By contrast, the relationship between fluoride ingestion and dental fluorosis remains clear, obvious, and easy to detect. In short, fluoridated water causes more damage to teeth than benefit. Accordingly, even if all other potential adverse effects are ignored (e.g., arthritis, bone fracture, brain damage, osteosarcoma, thyroid disease), the practice of fluoridating water fails a risk-benefit analysis on the subject of tooth quality alone.
Early Understandings
Fluoride’s ability to cause fluorosis was well known at the time U.S. health authorities endorsed water fluoridation in the 1950s. At that time, however, health authorities believed that fluoridating water at 1 part per million (ppm) would have very little effect on fluorosis rates, but a very large effect on tooth decay.
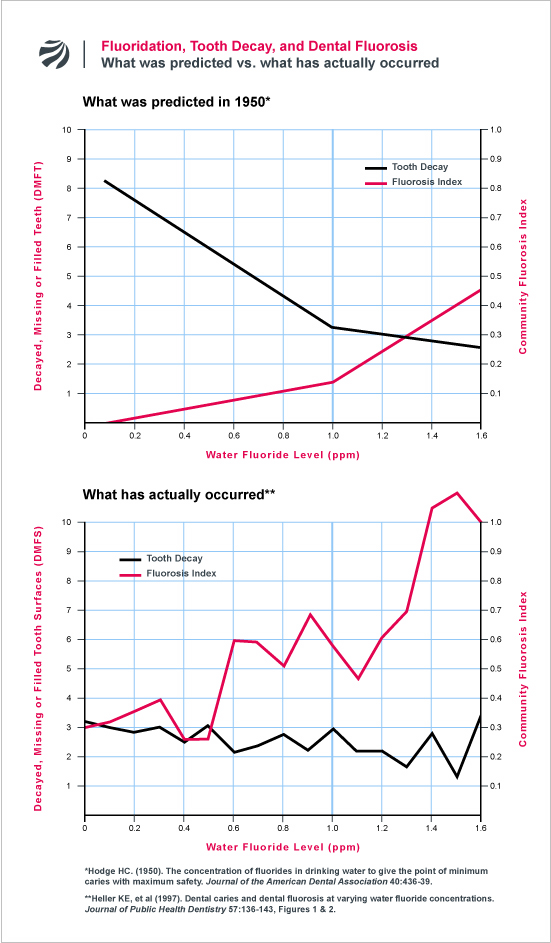
In a seminal paper published in 1950, Dr. Harold Hodge produced a figure that illustrated the predicted effect that fluoridation would have on both tooth decay and dental fluorosis. Hodge’s figure, which is reproduced below, estimated that as the fluoride level in water was increased from 0 to 1 ppm, the tooth decay rate would plummet by over 60%, while the fluorosis rate would only marginally increase. Based on this calculation, Hodge concluded that fluoridation could reduce tooth decay without a trade-off of increased fluorosis. He thus recommended that dentists and doctors show the figure to patients who were concerned about fluoridation to assure them of the program’s safety and efficacy. As Hodge wrote:
“If a patient comes into the office with a series of questions about fluorides, the busy practitioner might not have at his finger tips a quick, easily grasped answer. Suppose the patient asks how much good fluorides will do if they are put in the drinking water and how we know that they are safe. Answers can be given briefly and convincingly by a little sketch made of two straight lines.”
Current Understandings
Hodge’s predictions have not aged well. Research spanning from the 1980s to the present has demonstrated that the risk-benefit equation vis-a-vis dental fluorosis and tooth decay is far different than what Hodge and U.S. health authorities had estimated. Indeed, current data shows the opposite of what was predicted: namely, raising the fluoride level in water from 0 to 1 ppm has little measurable effect on tooth decay, but has a large and significant effect on dental fluorosis.
Consider, for example, the following two studies:
1. NIDR’S 1986-87 NATIONAL ORAL HEALTH SURVEY
In the 1980s, the National Institute of Dental Research (NIDR) conducted a national survey of oral health among U.S. schoolchildren. As part of this survey, NIDR dentists not only examined the teeth of over 39,000 children for signs of tooth decay and dental fluorosis, but also collected detailed history about the fluoride levels in each child’s home water supply from birth to the time of the exam. When pro-fluoride researchers from the University of Michigan crunched these numbers and displayed them graphically, the results looked far different from what Hodge had predicted. The following figure contrasts Hodge’s prediction with the results of the NIDR survey:
As can be seen, the NIDR study found that the community fluorosis index (CFI) at 1 ppm was almost five times higher than Hodge had predicted (~0.6 vs. ~0.14). By contrast the reduction in tooth decay was barely evident. Whereas Hodge had predicted that 1 ppm fluoride would reduce decay by over 60%, the NIDR’s analysis found that 1 ppm fluoride reduced decay by only about 18%. What makes this difference particularly striking is that the predicted reduction in tooth decay in Hodge’s figure was based on the cruder DMFT index (where benefits are much harder to detect), whereas the NIDR’s analysis was based on DMFS (a more sensitive measure where benefits are much easier to detect). The Michigan team’s analysis demonstrates, therefore, that the risk/benefits of water fluoridation with respect to teeth is far, far different that was estimated to be the case when fluoridation began.
2. IOWA FLUORIDE STUDY (1990’S-2000’S):
Following publication of the NIDR’s findings, dentists dismissed the significance of the results by claiming that the reduced effectiveness of fluoridation was simply because of the increased use of fluorides in dentistry as well as the “multiplier effect” where children in non-fluoridated areas are exposed to fluoridated drinking water through processed beverages, etc. This idea, however, has been seriously challenged by the results of an NIH-funded, multi-million dollar, decades-long study carried out by researchers at the University of Iowa.
Known as the “Iowa Fluoride Study,” the aim of the study was to monitor the fluoride intake of a group of children from birth to adolescence in order to determine to what extent total fluoride ingestion from all sources is associated with tooth decay and dental fluorosis. Under the “multiplier effect” theory, the more fluoride the children were exposed to, the lower their rate of tooth decay should be. However, in 2009, the Iowa researchers reported that total daily intake of fluoride from birth through adolescence had no significant relationship to whether the children developed any cavities in their teeth. By contrast, total fluoride intake was significantly related to whether the children developed dental fluorosis. According to the authors:
“These findings suggest that achieving a caries-free status may have relatively little to do with fluoride intake, while fluorosis is clearly more dependent on fluoride intake.”
SOURCE: Warren J, et al. (2009). Considerations on optimal fluoride intake using dental fluorosis and dental caries outcomes: A longitudinal study. Journal of Public Health Dentistry 69:111-15.