Research Studies
Study Tracker
Children’s Oral Health Initiative program’s impact on First Nations and Inuit children.Abstract
Objective:
To review data from the Children’s Oral Health Initiative (COHI) database from 2006 to 2016 to determine the impact of COHI on the oral health of registered First Nations and Inuit children in Atlantic Canada (AC), Saskatchewan, and Ontario.
Methods:
Data from the national COHI database were analysed for children ages 0 to 7 years in participating Indigenous communities. The mean age of participants and the number of children participating in COHI, receiving a first dental screening, fluoride varnish applications, sealants, and atraumatic restorative therapy were evaluated. Participants were grouped into 3 age categories (0–2, 3–5, 6–7). The decayed, extracted, and filled primary teeth (deft) scores were calculated.
Results:
Between 2006 and 2016, 80,574 children with an average age of 3.8 ±2.2 years participated in COHI in Saskatchewan, Ontario, and AC. The proportion receiving oral screenings, fluoride varnish, and sealants remained consistent over time. From 2006 to 2012, the number of participants receiving atraumatic restorative therapy increased in Saskatchewan and AC, and deft scores remained relatively stable with a marginal increase observed. This finding coincided with advancing age of children in all regions. Comparison of mean deft scores for children ages 0 to 7 years between 2006–2011 and 2012–2016 revealed an increase in Ontario and Saskatchewan. In AC, there was a significant decline in mean deft scores over the 2 time periods.
Conclusion:
While no significant decreases in deft scores were identified, the findings suggest that children participating in COHI are receiving needed preventive services such as fluoride varnish and atraumatic restorative therapy.
Practical Implications of This Research.
- The evaluation of COHI data provides evidence of its impact on the oral health of First Nations and Inuit children. Decision makers can use this information to strategically refine services, tailoring them to diverse community needs for greater responsiveness and impact.
- These findings guide decisions on COHI’s continuity, modification, or expansion, emphasizing its significance in customizing oral health strategies to the unique requirements of First Nations and Inuit communities.
There is a disproportionately higher level of early childhood caries (ECC) in the primary teeth of Canadian Indigenous (First Nation, Inuit, and Métis) children under 6 years of age. The prevalence of ECC in some Canadian Indigenous communities is over 90%.1 The 2010 Indian Health Service Oral Health Survey of American Indian and Alaskan Native (AI/AN) Preschool Children reported similar findings, with 75% of AI/AN children experiencing dental decay by age 5.2 Many risk factors are associated with ECC, including poverty, household crowding, family size, nutrition, health behaviours, parenting practices, and the caregiver’s oral health. For Indigenous children living on federal reserves, which are often geographically isolated, and in remote communities, access to oral health care is substantially limited.3 Unsurprisingly, children from such communities have a higher caries burden, often measured by caries indices such as the decayed, extracted, and filled primary tooth (deft) index.
The Children’s Oral Health Initiative (COHI) began in 2004 as a federally funded, population-based oral health prevention program in Canada to reduce the prevalence of dental caries for First Nations and Inuit children living on federal reserves and in remote communities in Canada.3 The goal of COHI is to improve access to preventive oral health services and shift the emphasis from a primary treatment-based approach (i.e., surgical/restorative care) for caries to a more balanced primary prevention and conservative treatment focus (i.e., oral health education, annual oral health screenings, fluoride varnish applications, sealants, and temporary fillings).3,4 The target groups of the COHI program are children ages 0 to 7, parents/primary caregivers, and pregnant women.3 This population health program addresses the oral health inequities that exist for First Nations and Inuit children to improve their oral health outcomes.3
Depending on the province, COHI is delivered in communities by either a dental therapist or a dental hygienist, along with the assistance of COHI aides, community members hired and trained to assist the oral health care professional.3, 5 The COHI aide is a key component of the program as the COHI aide offers community-based and community-engaged support and assistance in connecting the dental therapists and dental hygienists with the community to provide oral health services. 3 Preventive oral health care services provided by COHI include fluoride varnish (FV) applications, sealants, atraumatic restorative treatment (ART), and oral health counselling.6 It is important to note that, in Ontario, the scope of practice does not permit dental hygienists to perform ART.
There are more than 630 First Nations and 53 Inuit communities in Canada.7 According to Health Canada, in 2016, COHI was provided in 238 of 452 eligible First Nations and Inuit communities. 8 Since 2014, COHI has been administered in British Columbia (BC) by the BC First Nations Health Authority. Therefore, data for the province of BC are not included in the national total of First Nations communities participating in COHI.3
The purpose of this study was to analyze data from the national COHI database from 2006 to 2016 and to determine the impact that COHI is having on the oral health of registered First Nations and Inuit children participating in COHI in Atlantic Canada, Saskatchewan, and Ontario. As of 2014, COHI exists in 32 of 34 First Nations communities in Atlantic Canada, 69 of 139 First Nations communities in Ontario, and 42 of 70 First Nations communities in Saskatchewan.3
Ethics approval for this research was provided by the University of Manitoba’s Health Research Ethics Board (HREB). The research team received appropriate permissions from the National COHI office in the Department of Indigenous Services Canada, along with the First Nations and Inuit Health Branch (FNIHB) offices in the 3 regions: Atlantic Canada (New Brunswick, Newfoundland and Labrador, Nova Scotia, and Prince Edward Island), Saskatchewan, and Ontario to undertake an analysis of the data of COHI services delivered in each region.
Data source and measures
COHI data were provided from the national COHI program database maintained by the Department of Indigenous Services Canada. Data were provided for Atlantic Canada, Ontario, and Saskatchewan, which represents 6 of 10 Canadian provinces. In keeping with the study’s agreement with the Department of Indigenous Services Canada and the respective First Nations and Inuit Health Branch (FNIHB) regions, no comparisons were made between regions.
A multidisciplinary team evaluated the COHI data. Quantitative analyses were undertaken for each of the 3 regions. The analysis explored the preventive services provided by COHI staff and determined the yearly proportion of children receiving their first dental visit by the recommended 12 months of age and first screenings for all ages (0 to 7 years), first and second FV applications, dental sealants, and ART. First visits were assessed in 2 ways: the proportion of first screenings in all ages (0 to 7 years) and the proportion of first visits by age 12 months. This was done to compare the proportion of children receiving their first screening by the recommended 12 months of age to the proportion of those visiting for the first time in general (0 to 7 years). The trends in these preventive services over time (2006 to 2016) were analysed. The prevalence of total caries experienced and cumulative counts of the number of decayed, extracted due to caries, and filled primary teeth (deft) scores were assessed. An analysis of changes in prevalence and caries scores over time was undertaken to determine trends. Participants were divided into 3 age groups: 0–2 years, 3–5 years, and 6–7 years.2 Comparisons of mean deft scores for children ages 0 to 7 years for each region were also performed between the first 6-year period of COHI data (2006–2011) and the second 5-year period (2012–2016).
Statistical analysis
Data were provided as an Excel spreadsheet and analyzed using Number Cruncher Statistical Software NCSS Version 9 (Kaysville, Utah). Statistical analysis included descriptive statistics (frequencies, means, ± standard deviations [SD]) and bivariate analysis (two-sample t-test). Simple comparisons of deft scores between 2006 and 2016 were performed by 2-sample t-test analyses for each age category at the start and end of the 11-year data period. Additionally, mean deft scores for the first 6 years were compared to the mean deft scores for the last 5 years in each region. A p value <0.05 denoted significance.
In total, 80,574 children from all 3 regions participated in the COHI program from 2006 to 2016 (Table 1). The average number of children ages 0 to 7 years participating annually was 7,324, with 2006 having the least number of children participating (4,773) and 2013 having the highest number of children participating (8,755) (Table 1). Looking at the first 6 years of the study (2006 to 2011), the average yearly number of children participating in COHI was 6,581 ±1,173 compared to the average yearly number of children participating in the last 5 years of the study (2012 to 2016), which was 8,218 ±604. There was a significant statistical difference in the number of children participating in COHI between the first and second time periods (p = 0.036). The mean age of COHI participants across the years under investigation was 3.8 ±2.3 years (Table 2).
First screenings
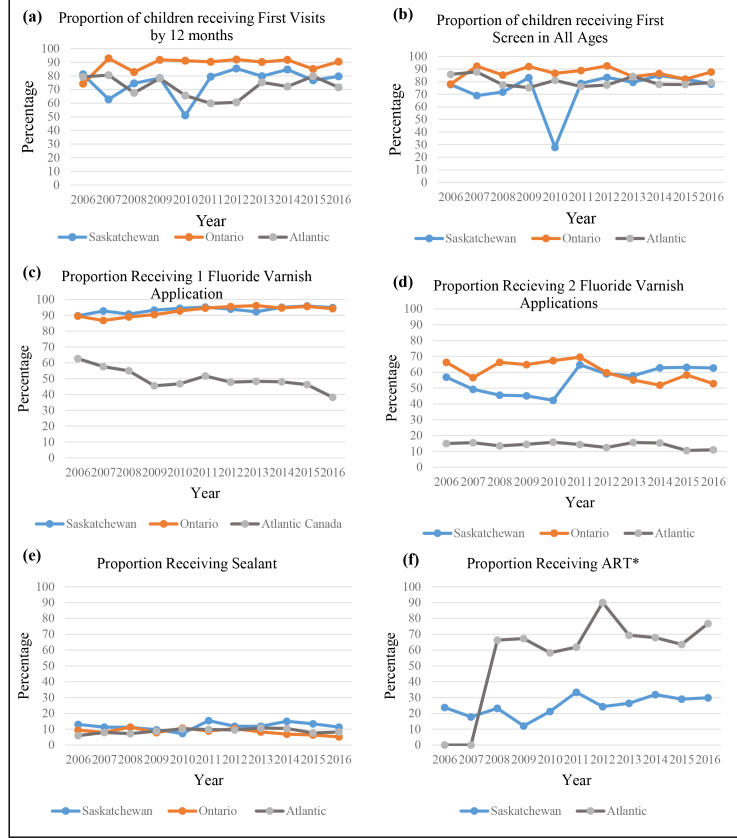
The proportion of children receiving first visits by 12 months of age and the proportion receiving first screenings in all years (0 to 7 years) are presented in Figures 1A and 1B. The proportion of first screenings for all years was relatively consistent throughout the study period, ranging from 75.2% to 92.5%. The proportion of first visits by 12 months of age was mostly consistent but demonstrated a slightly wider fluctuation than the first screening for all years (62.3% to 94%). A considerable reduction in the proportion of children receiving first visits and first screenings in 2010 in Saskatchewan was observed. There was a statistically significant difference when comparing the first screenings for all ages in all regions to the first visits by age 12 months (p = 0.0055).
In Atlantic Canada, the mean percentage of first visits by 12 months of age was 71.9% ±7.6%, and the mean percentage of screening in all ages was 80.0% ±4.2%. In Saskatchewan, the mean percentage of the first visit by 12 months of age was 75.8% ±10.2% and the mean percentage of screening in all ages was 74.2 ±16.1%. In Ontario, the mean percentage of the first visit by 12 months of age was 88.4% ±5.6% and the mean percentage of screening in all ages was 86.9 ±4.5%. Overall, COHI screened 6,946 children by 12 months of age, while 64,857 children ages 0 to 7 years received a first screening in all 3 regions over the study period (2006 to 2016).
Fluoride varnish
The proportions of children receiving first and second FV applications as part of COHI are presented in Figures 1C and 1D. The proportion of first FV applications remained consistent over the study years, with mean percentages being 93.5% ±2.0%, 92.7% ±3.2%, and 49.8% ±6.6% in Saskatchewan, Ontario, and Atlantic Canada, respectively. However, the percentage of children from COHI communities receiving a second FV application was significantly lower ( p < 0.05) in all 3 regions, with mean percentages over the study years being 55.4% ±7.9%, 60.8% ±6.3% and 14.0% ±1.9% in Saskatchewan, Ontario, and Atlantic Canada, respectively.
Table 1.
Number of COHI participants in Atlantic Canada, Ontario, and Saskatchewan over the study period
| Region | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Atlantic Canada | 1230 | 1166 | 1158 | 1248 | 1463 | 1890 | 1936 | 1918 | 1949 | 1812 | 1697 | 17467 |
| Ontario | 1064 | 1791 | 2611 | 2784 | 2982 | 2990 | 2992 | 3263 | 3312 | 2648 | 2745 | 29182 |
| Saskatchewan | 2479 | 2702 | 3006 | 2621 | 2631 | 3668 | 3406 | 3574 | 3435 | 3403 | 3000 | 33925 |
| Total | 4773 | 5659 | 6775 | 6653 | 7076 | 8548 | 8334 | 8755 | 8696 | 7863 | 7442 | 80574 |
Table 2.
Mean age of children (years) participating in COHI by region and program year
| Region | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Atlantic Canada | 4.21 | 4.32 | 4.34 | 4.06 | 4.28 | 3.96 | 3.95 | 4.05 | 4.16 | 4.33 | 4.28 |
| Ontario | 3.83 | 3.57 | 3.51 | 3.48 | 3.53 | 3.58 | 3.61 | 3.70 | 3.92 | 4.08 | 4.03 |
| Saskatchewan | 3.70 | 3.71 | 3.61 | 3.80 | 3.48 | 4.88 | 3.49 | 3.50 | 3.64 | 3.71 | 3.70 |
Figure 1.
Sealants
Figure 1E shows that the proportion of children having sealants was low compared to other COHI services over the study period, ranging between 7.3% and 15.4% in Saskatchewan, 5.2% and 11.3% in Ontario, and 5.9 and 10.7% in Atlantic Canada. It also remained consistently low throughout the program years in all 3 regions.
Atraumatic restorative therapy
The proportion of children receiving ART was examined over the study period (Figure 1F). No data were available for Ontario as scope of practice does not permit dental hygienists to perform ART in that province. In Atlantic Canada the proportion of children receiving ART ranged from 0% to 90.0% over the study period, while children receiving ART in Saskatchewan ranged from 12.2% to 33.4%.
Decayed, extracted, and filled teeth (deft) index scores
Children’s deft scores for all 3 regions were calculated and potential changes in deft scores were investigated over the study period (Figure 2). Overall, there were no significant changes in deft scores over time in Saskatchewan, Ontario, and Atlantic Canada (p = 0.64, p = 0.71, and p = 0.86, respectively). The trend lines for the 3 age groups (0–2 years, 3–5 years, and 6–7 years) stayed relatively stable in all 3 regions, except for a sharp decline in 2010 deft scores in Saskatchewan for children 3 years of age and older, corresponding to the drop in COHI screening activity in Saskatchewan that year for children 3 years of age and older followed by a drastic increase in enrollment in 2011. Comparison of mean deft scores for children ages 0 to 7 years during the first 6 years (2006–2011) and the last 5 years (2012–2016) revealed a significant increase from the first time period to the second time period in Ontario (4.75 versus 5.05, p < 0.0001). A significant increase was also observed when comparing mean deft scores for those same time periods in Saskatchewan (3.57 versus 4.61, p < 0.0001), even after removing data for 2010 (4.03 versus 4.61, p < 0.0001). However, comparisons of mean deft scores for children ages 0 to 7 years in Atlantic Canada during the first 6 years (2006–2011) and the last 5 years (2012–2016) revealed a significant decline from the first time period to the second time period (3.09 versus 3.0, p < 0.0001).
This evaluation of COHI program data provides evidence that COHI is having a positive impact on the oral health of children in COHI communities in Atlantic Canada, Ontario, and Saskatchewan, as registered First Nations and Inuit children participating in the program are receiving much-needed preventive oral health services. While the goal, mission, and vision of COHI are standard nationally, the way in which the COHI program is delivered across Canada varies between regions as does administrative tracking. For example, there are differences in provincial and territorial oral health provider regulations. In many regions, COHI is delivered by dental therapists, while in provinces such as Ontario and Quebec, the clinical services are delivered by dental hygienists. These regulatory differences result in some preventive services (e.g., ART) not being tracked in the same manner and being absent from the national COHI program database for some regions. While dental hygienists working for COHI in Ontario are unable to perform ART and record ART in the COHI database, they are performing “interim stabilization treatment,” which is a modified version of ART. Future tracking of interim stabilization treatments will provide a more complete picture of COHI services. When looking at the COHI delivery differences, it is crucial to exercise caution before attributing them solely to regulatory factors. It is tempting to point to regulation as a primary driver, but the presence of numerous intricate contextual, regional, and geographic nuances that may elude the scope of this study cannot be ignored.
Professional oral health organizations all recommend that children’s first oral health visit should occur no later than 12 months of age or within 6 months after a child’s first tooth erupts.9, 10 Offering an inviting dental home early and getting children and their caregivers into the oral health environment and system from a young age helps establish trust and preventive oral health routines for life.10–12 COHI aims to create the opportunity for registered First Nations and Inuit children to access culturally safe preventive oral health care.4 The decline in first visits in Saskatchewan in 2010 relates to a temporary reduction in COHI service providers and COHI activities that year.
Unfortunately, not every young child receives timely first visits in keeping with professional recommendations, as data from one urban population in Canada showed that <2% of those under 2 years of age had a first dental visit.11 Thankfully, other Canadian data point to greater awareness of and access to early first dental visits for infants and toddlers (e.g., Manitoba Dental Association’s Free First Visit program). 13– 15 While COHI numbers for first oral health screenings are much higher than what has been reported for children in Toronto, continued improvements in access to preventive oral health care for young Indigenous children through COHI must be sustained. It is critical that First Nations and Inuit children from rural and remote communities have the ability to meet these early preventive oral health assessment milestones.11 Further or future studies could solicit input from parents/primary caregivers and pregnant women, as they are also target groups of COHI.
Figure 2.
FV is an evidence-based topical therapeutic treatment to help reduce the risk for caries and prevent further caries development.16, 17 Children who are at high risk for caries benefit from regular FV applications—a minimum of 2 applications per year to reduce caries risk.16 The COHI data revealed that over 90% of eligible children received a one-time FV application, but a considerable proportion of children did not receive 2 FV applications. Fluoride was applied by COHI oral health care providers, but caries risk assessments and the subsequent FV applications could also be applied, with limited training, by non-oral health care providers.18
Fewer second applications of FV in all regions may be a result of COHI provider and staffing issues and challenges and not having the resources to provide this important preventive service. If oral health services are not consistently available in remote First Nations communities, collaborating with health care providers in the community and providing them with the skills to assess caries risk and apply FV could greatly increase the number of children receiving regular FV applications and in turn decrease deft scores.19, 20 It is also possible that there was community hesitancy in receiving either a first or second FV application or the children were receiving this oral health preventive intervention outside of the COHI program. The Non-Insured Health Benefits (NIHB) program provides coverage for dental care to eligible First Nations and Inuit patients, whether within or outside their communities. In contrast, COHI exclusively operates within communities. It is worth noting that oral health services may have been administered by non-COHI oral health providers, and therefore not tracked through COHI.
Sealant placement is recommended on children’s primary and permanent molars to control and prevent caries.21, 22 Sealants reduce the risk of developing caries and the future need for invasive restorations by acting as a physical barrier to prevent biofilm accumulation in those difficult-to-clean occlusal pits and fissures.21 Preventive oral health behaviours such as brushing teeth twice a day with fluoridated toothpaste and reducing the frequency and number of cariogenic snacks combined with sealant placement can further reduce the risk of caries development.10, 21 In the current study, the proportion of one-time sealant placements remained consistent throughout the study years as COHI aides helped schedule appointments for sealant placements. However, the overall proportion of COHI participants receiving sealants is low. Despite the evidence that sealants are efficacious at preventing and controlling caries, 22, 23 the COHI data correlate to the overall trend that sealants are underused. The majority of COHI participants receiving sealants were in the age range of 5 to 7 years. The mean COHI participant age range from all 3 regions was 3.5 to 4.9 years (Table 2), which might account for overall low proportion of children receiving sealants. One reason for this may be because many oral health professionals still view sealants as a preventive treatment for permanent molars, thereby not considering it for primary molars in children under 6 years of age. Age, cooperation of the child, and an unfamiliar environment for the procedure are potential barriers for sealant placements across all ages, but particularly for younger COHI participants.17 Another reason is that many insurance programs do not reimburse oral health care providers for placing sealants on primary molars. For these reasons the oral health care providers might have been hesitant to place sealants on primary teeth.
ART is a restorative technique used to treat caries in populations where access to professional oral health care is challenging.24 It is a minimally invasive approach, which involves the removal of decay with hand instruments followed by the placement of a temporary filling, usually glass ionomer.24, 25 For children in remote communities, ART is an acceptable approach to managing caries as it assists in addressing caries lesions.24– 27 In Saskatchewan 28and Atlantic Canada, COHI services are provided by dental therapists wher,e ART is included in their scope of practice.28 It is reasonable to see an increase in the use of ART in Atlantic Canada and Saskatchewan, given the correlation with an increased number of service providers who can offer ART in those remote First Nations and Inuit communities. Dental therapists are not part of the COHI program in Ontario because they do not practise in that province. In Ontario, COHI functions through the services provided by dental hygienists who can place temporary restorations as part of their scope of practice, but it is referred to as interim stabilization therapy (IST) and is not tracked in the national COHI database.29 As a result, there is no data for ART in Ontario.
Implementing the use of silver diamine fluoride (SDF)30 as an additional COHI service to treat cavitated lesions would assist in the non-restorative management of decayed teeth without the oral health care provider scope of practice regulation discrepancies. SDF acts to arrest decay and prevents the incidence of new carious lesions. The treatment does stain the decay, turning it black. Therefore, caution needs to be taken when using SDF to ensure the caregiver understands its aesthetic consequences and provides consent.31 COHI has now begun to introduce SDF as a recognized non-restorative caries management technique.
The presence of COHI in the communities and its ability to increase access to oral health care and preventive services have impacted the deft scores in children ages 0 to 7 years. The deft scores in all regions follow a similar trajectory, remaining consistent across the study period and age categories. The deft scores account for both treated and untreated decay. The data show that trends in preventive care treatments (initial screenings, first and second fluoride applications, sealant applications, and ART where tracked) remained consistent over the study period, implying COHI services are assessing and addressing treated and untreated decay. Future improvements in deft scores are possible with continued COHI presence in the communities, with additional health care provider collaboration, and a focus on related determinants of health, such as strategies to improve access to food that promotes healthy growth and development.
Even though COHI data do not demonstrate a dramatic downward trend in deft scores, children having access to and receiving consistent preventive oral health care is a step in the right direction to improve the oral health status of COHI participants. These conclusions are similar to a study assessing 5-year results of the American Indian Health Service Early Childhood Collaborative.2 This initiative looked at increasing access to dental care and preventive oral health care services for Indian/Alaskan Native preschool children.2 It was found that oral health prevention strategies resulted in an initial improvement in the oral health status of children and a lower prevalence of decay, especially for 1- to 2-year-olds.2
The Interim Canada Dental Benefit for children under the age of 12 and the Canadian Dental Care Plan (CDCP) for uninsured and under-insured low- and middle-income families are also steps in the right direction.32, 33 The CDCP program will address needs from a therapeutic/treatment perspective. However, the continued work of COHI to promote preventive oral health care services will create opportunities for more registered First Nations and Inuit children to have a healthy oral future.
While the data demonstrate that COHI services are helping, the COVID-19 pandemic has inevitably affected the oral health of First Nations and Inuit children who would have participated in COHI during those years. It is likely that there have been setbacks in some of the progress made by COHI for specific oral health milestones such as first visits, FV applications, ART, and sealants. Further research is needed to analyse COHI experiences during COVID, and additional resources may be required to increase numbers to where they were prior to the pandemic and beyond.
Limitations
This study is not without limitations. This present assessment evaluated program outcomes for select regions and COHI communities across Canada. Each region and COHI community is unique, making it impossible and unethical to compare regions and communities. There is also the potential for lack of calibration between COHI programs in each community. Each COHI provider (dental hygienist or dental therapist) and COHI aide may deliver the program differently in their community based on the individual needs of those community members and COHI participants. Given differences in levels of community resources and structural supports, there may be some minor differences in how the COHI program is delivered across all participating communities in Canada, which may also impact the positive effect of the COHI program.
Additional regional COHI data were not part of the national COHI repository data and could not be included in the study. There may be administrative, regional, cultural, and geographic disparities not present in the data alone that should be considered. These considerations should not only inform current understanding, but also serve as valuable insights for future studies and data collection endeavours, prompting a more nuanced exploration of the multifaceted influences shaping the landscape under examination. For example, the regulations in Ontario governing ART and IST resulted in temporary restoration services not being tracked in Ontario. This gap in the data makes it difficult to track preventive services within COHI and their potential impact on COHI participants. The COHI data also do not track participants referred for advanced dental treatment requiring general anesthesia. This would be helpful information to collect as it would permit investigating whether the implementation of a preventive oral health program, such as COHI, in a community contributes to a decline in the need for extensive dental treatment requiring general anesthesia. Information about the workforce would also be helpful to evaluate if the stability of trends could be due to workforce limitations.
With the high prevalence of dental caries and other oral disease in children in remote First Nations and Inuit communities, COHI is a beneficial resource, encouraging early intervention and increasing access to preventive oral health care services. The evaluation of COHI data and services delivered provides evidence of the relevance and impact of COHI on First Nations and Inuit children and their families. Regional variations emerged between 2006–2011 and 2012–2016, highlighting noteworthy regional differences in oral health outcomes over time. Although statistical analyses were not undertaken in this study to compare regional datasets, the trends in regional differences in oral health outcomes over time warrant further exploration. This is important as findings may inform decision making around continuing, modifying, and expanding COHI to more First Nations and Inuit communities. The data do not show significant decreases in deft scores. However, the consistency of first oral health screenings and the oral health preventive services offered in these communities prevent a significant increase in deft scores.
With further expansion of the COHI program into more First Nations and Inuit communities and more dental hygienists, dental therapists, and COHI aides participating in the program, it is essential to blend the proven preventive strategies with First Nations and Inuit cultural approaches. Knowledge and capacity sharing approaches such as Two-Eyed Seeing to build and strengthen relationships between program providers and communities will have a greater impact on oral health for all future generations.34
The authors have no conflicts of interest to declare.
The authors express sincere gratitude to the following organizations and individuals for their contributions to this research: Canadian Institutes of Health Research, University of Manitoba, Dalhousie University, and Dr. Vivianne Cruz de Jesus.
CDHA Research Agenda categories: risk assessment and management; access to care and unmet needs
- Pierce A, Singh S, Lee J, Grant C, Cruz de Jesus V, Schroth RJ The burden of early childhood caries in Canadian children and associated risk factors Front Public Health 2019; 7: 328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricks TL, Phipps KR, Bruerd B The Indian Health Service Early Childhood Caries Collaborative: A five-year summary Pediatr Dent 2015; 37( 3): 275- 280 [PubMed] [Google Scholar]
- Mathu-Muju KR, McLeod J, Walker ML, Chartier M, Harrison RL The Children’s Oral Health Initiative: An intervention to address the challenges of dental caries in early childhood in Canada’s First Nation and Inuit communities Can J Public Health 2016; 107 (2): e188-e193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathu-Muju KR, McLeod J, Donnelly L, Harrison R, MacEntee MI The perceptions of first nation participants in a community oral health initiative Int J Circumpolar Health 2017; 76 (1): 1364960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroth RJ, Kyoon-Achan G, McNally M, Edwards J, White P, Tait Neufeld H, et al. Children’s Oral Health Initiative: workers’ perspectives on its impact in First Nations communities Health Promot Chronic Dis Prev Can 2023; 43 (9): 393- 402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathu-Muju KR, Kong X, Brancato C, McLeod J, Bush HM Utilization of community health workers in Canada’s Children’s Oral Health Initiative for Indigenous communities Community Dent Oral Epidemiol 2018; 46 (2): 185- 193 [DOI] [PubMed] [Google Scholar]
- Government of Canada. Indigenous and Northern Affairs Canada. rcaanc-cirnac.gc.ca/eng/1100100013791/1535470872302
- Office of the Auditor General of Canada. Report 4—Oral health programs for First Nations and Inuit—Health Canada. oag-bvg.gc.ca/internet/English/parl_oag_201711_04_e_42669.html
- Stijacic T, Schroth RJ, Lawrence HP Are Manitoba dentists aware of the recommendation for a first visit to the dentist by age 1 year? J Can Dent Assoc 2008; 74 (10): 903 [PubMed] [Google Scholar]
- Hale KJ, American Academy of Pediatrics Section on Pediatric Dentistry Oral health risk assessment timing and establishment of the dental home Pediatrics 2003; 111 (5 Pt 1): 1113- 1116 [DOI] [PubMed] [Google Scholar]
- Darmawikarta D, Chen Y, Carsley S, Birken CS, Parkin PC, Schroth RJ, et al. Factors associated with dental care utilization in early childhood. 2014 Pediatrics. 133(6):e1594. doi: 10.1542/peds.2013-3725. [DOI] [PubMed] [Google Scholar]
- Hachey S, Clovis J, Lamarche K Strengthening the approach to oral health policy and practice in Canada Paediatr Child Health 2020; 25 (2): 82- 85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroth RJ, Guenther K, Ndayisenga S, Marchessault G, Prowse S, Hai-Santiago K, et al. Dentists’ perspectives on the Manitoba Dental Association’s Free First Visit program J Can Dent Assoc 2015; 81: f21 [PubMed] [Google Scholar]
- Schroth RJ, Boparai G, Boparai M, Zhang L, Svitlica M, Jacob L, et al. Tracking early visits to the dentist: A look at the first 3 years of the Manitoba Dental Association’s Free First Visit program J Can Dent Assoc 2015; 81: f8 [PubMed] [Google Scholar]
- Alai-Towfigh H, Schroth RJ, Hu R, Lee VHK, Olatosi O Canadian dentists’ views on the first dental visit for children Front Oral Health 2022; 3: 957205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azarpazhooh A, Main PA Fluoride varnish in the prevention of dental caries in children and adolescents: a systematic review Tex Dent J 2008; 125 (4): 318- 337 [PubMed] [Google Scholar]
- Pollick H The role of fluoride in the prevention of tooth decay Pediatr Clin North Am 2018; 65 (5): 923- 940 [DOI] [PubMed] [Google Scholar]
- Khan SY, Schroth RJ, Cruz de Jesus V, Lee VHK, Rothney J, Dong CS, et al. A systematic review of caries risk in children <6 years of age Int J Paediatr Dent 2024; 34 (4): 410- 431 [DOI] [PubMed] [Google Scholar]
- Arif UA, Pitts E, Farrell C, Fontana M, Kinney JA Perception and utilization of oral screenings and fluoride application in medical offices following the Michigan Caries Prevention Program training J Dent Hyg 2021; 95 (1): 50- 56 [PubMed] [Google Scholar]
- Schroth RJ, Rothney J, Sturym M, Dabiri D, Dabiri D, Dong CC, et al. A systematic review to inform the development of a Canadian caries risk assessment tool for use by primary healthcare providers Int J Paediatr Dent 2021; 31 (6): 767- 791 [DOI] [PubMed] [Google Scholar]
- Naaman R, El-Housseiny A, Alamoudi N The use of pit and fissure sealants—a literature review Dent J (Basel) 2017; 5 (4): 34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright JT, Crall JJ, Fontana M, Gillette EJ, Nový BB, Dhar V, et al. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants: A report of the American Dental Association and the American Academy of Pediatric Dentistry J Am Dent Assoc 2016; 147 (8): 672- 682 e12 [DOI] [PubMed] [Google Scholar]
- Slayton RL, Urquhart O, Araujo MWB, Fontana M, Guzmán-Armstrong S, Nascimento MM, et al. Evidence-based clinical practice guideline on nonrestorative treatments for carious lesions J Am Dent Assoc 2018; 149 (10): 837- 849 e19 [DOI] [PubMed] [Google Scholar]
- Giacaman R, Muñoz-Sandoval C, Neuhaus K, Fontana M, Cha?as R Evidence-based strategies for the minimally invasive treatment of carious lesions: review of the literature Adv Clin Exp Med 2018; 27 (7): 1009- 1016 [DOI] [PubMed] [Google Scholar]
- Frencken JE Atraumatic restorative treatment and minimal intervention dentistry Br Dent J 2017; 223 (3): 183- 189 [DOI] [PubMed] [Google Scholar]
- Roberts-Thomson KF, Ha DH, Wooley S, Meihubers S, Do LG Community trial of silver fluoride treatment for deciduous dentition caries in remote Indigenous communities Aust Dent J 2019; 64 (2): 175- 180 [DOI] [PubMed] [Google Scholar]
- Holve S, Braun P, Irvine JD, Nadeau K, Schroth RJ, et al. Early childhood caries in Indigenous communities Paediatr Child Health 2021; 26 (4): 255- 258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saskatchewan Dental Therapists Association. What Is a Dental Therapist? sdta.ca/about/history.html
- College of Dental Hygienists of Ontario. Guideline: Placement of temporary restorations. cdho.org/docs/default-source/pdfs/reference/guidelines/placementtemprestorations.pdf
- Urquhart O, Tampi MP, Pilcher L, Slayton RL, Araujo MWB, Fontana M, et al. Nonrestorative treatments for caries: systematic review and network meta-analysis J Dent Res 2019; 98 (1): 14- 26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyoon-Achan G, Schroth RJ, DeMaré D, Sturym M, Edwards J, Lavoie JG, et al. Indigenous community members’ views on silver diamine fluoride to manage early childhood caries J Public Health Dent 2020; 80 (3): 208- 216 [DOI] [PubMed] [Google Scholar]
- Canadian Dental Hygienists Association. The new Interim Canada Dental Benefit information for dental hygienists. cdha.ca/cdha/The_Profession_folder/Canada_Dental_Benefit/CDHA/The_Profession/Canada_Dental_Benefit/Canada_Dental_Benefit.aspx
- Schroth RJ, Cruz de Jesus V, Menon A, Olatosi OO, Lee V, Yerex K, et al. An investigation of data from the first year of the interim Canada Dental Benefit for children <12 years of age Front Oral Health 2024; 4: 1328491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin DH Two-eyed seeing: A framework for understanding Indigenous and non-Indigenous approaches to Indigenous health research Can J Nurs Res 2012; 44 (2): 20- 42 [PubMed] [Google Scholar]