Fred Pearce travels to central India to unravel the origins of a crisis now threatening tens of millions of people worldwide
The pump was installed in Shatap’s village of Hirapur, in the central Indian state of Madhya Pradesh, during the UN’s International Water Decade of the 1980s. Its borehole was one of millions sunk worldwide in a highly publicised race to provide the world’s poor with “safe” drinking water, planned and part-funded by aid agencies such as the UN children’s fund, Unicef. The underground water was indeed mostly free of the bacteria that can infest polluted surface water. But nobody ever tested the underground water for natural chemicals, such as fluoride, even though they were known to be widely present in rocks from which the water was pumped.
 Madhya Pradesh itself is famous for its rich mineral deposits. “The problem is enormous, unbelievable,” says Andezhath Susheela of the Fluorosis Research and Rural Development Foundation in Delhi. She has been unravelling the national story for a decade during which time her estimate of the number of people leading “a painful and crippled life” from fluorosis has risen from one million to 25 million and now to 60 million – six million of them children – spread across tens of thousands of communities. “In some villages three-quarters of the population are seriously affected.”
Madhya Pradesh itself is famous for its rich mineral deposits. “The problem is enormous, unbelievable,” says Andezhath Susheela of the Fluorosis Research and Rural Development Foundation in Delhi. She has been unravelling the national story for a decade during which time her estimate of the number of people leading “a painful and crippled life” from fluorosis has risen from one million to 25 million and now to 60 million – six million of them children – spread across tens of thousands of communities. “In some villages three-quarters of the population are seriously affected.”
Meet 10-year-old Shatap, with a walk straight out of Monty Python. But this diminutive figure is not playing games as he waddles up the muddy lane, his knees locked together and his stunted and misshapen lower legs splayed wide like flippers. His gait is permanent; his bones grossly deformed by fluoride in drinking water pumped from a borehole at the bottom of the lane.
The first rains of this summer’s monsoon are beginning to fall as Shatap and his friends assemble in the yard of the Hirapur village head, Chudaman Bhavre. Almost all of them are knock-kneed and have the brown-stained teeth characteristic of the first stages of fluoride poisoning. They drank water from a poisoned pump while attending the village primary school close by. Fluoride levels in the water were 11 times the safety limit of one part per million.
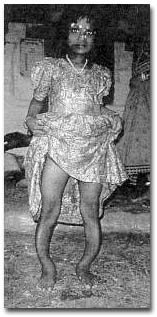
Krishna looks nine years old. She is 14. She cannot walk to school because her legs are cruelly bowed by fluorosis.
The children who lived nearest to the pump and drank its water continuously have suffered most. Besides Shatap, there is Kamala and her bow-legged sister Krishna, both daughters of the village head. Aged 14 but looking no more than nine, Krishna was forced to abandon schooling because her deformed limbs could no longer take her to the secondary school in a neighbouring village.
 Many parents, including Krishna’s mother, suffer painful, stiff and misshapen backs and hips, and chronic gastro-enteritis. Bhaskar Raman, a local activist who brought the village’s plight to the attention of doctors, says there has been an epidemic of stillbirths and involuntary abortions – all known symptoms of fluoride poisoning.
Many parents, including Krishna’s mother, suffer painful, stiff and misshapen backs and hips, and chronic gastro-enteritis. Bhaskar Raman, a local activist who brought the village’s plight to the attention of doctors, says there has been an epidemic of stillbirths and involuntary abortions – all known symptoms of fluoride poisoning.
All across Mandla, a district of a million or so people in eastern Madhya Pradesh, a steady stream of children have reported similar complaints since the late 1980s. But in this remote corner of central India, doctors hadn’t heard of fluorosis. They instead diagnosed arthritis, polio, rickets, a genetic fault or simply a “mystery disease”. The link with water was never made.
Until, that is, Tapas Chakma, a young research officer at the Regional Medical Research Centre in Jabalpur came to the village of Tilaipani in 1995 and suggested that a local girl’s strange disease might be fluorosis. Initially, he was rebuffed by local officials. “I asked the Pollution Control Board about the water here, and they assured me it was safe,” Chakma recalls. “I didn’t accept that and sent a water sample to Delhi, which revealed the truth.” Soon he began to hear about other villages with similar problems, and he demanded a district-wide screening of water.
Three years later, engineers have dismantled more than 500 pumps in more than 300 villages in Mandla to prevent people drinking the poisoned water. Chakma’s boss at the medical research centre, Ravi Shankar Tiwary, says “some of the blame lies with aid agencies such as Unicef”. These bodies lobbied for and helped fund the boreholes-and-handpumps programme. “But I also blame the public health engineers in Mandla for what has happened. They dug the wells. They said at first that they had tested the water. But they didn’t. I know. They didn’t have the right equipment.”
The whiff of corruption hangs over the Mandla story. Raman alleges that private contractors sank boreholes deeper than necessary as part of a scam to milk the public purse. He says that 30 metres would have been deep enough – a figure borne out now, at the end of the dry season, when open wells in the villages contain water at depths of between just 15 and 20 metres. Sinking the boreholes to 50 metres increased the value of the contracts, Raman says, but it also penetrated the fluoride-bearing rocks that were only present at these lower depths.
Officials at the Mandla department of public health engineering brush off inquiries, even from Unicef, which has sought to repair damage by offering to install some trial defluoridation equipment. “In Mandla, the administration is so terrified they won’t let us go near,” says Vishwas Joshi, Unicef’s water project officer in Delhi.
But Mandla’s tragedy is a tiny part of a vast landscape of ignorance, confusion and indifference that is crippling millions in the state of Madhya Pradesh and beyond. A decade ago, government scientists named 12 districts in the state, including Mandla, as being at risk from fluoride in water. To date, only Mandla’s wells have been fully surveyed. But the more the scientists look, the more they find. Just last month, dozens of pumps were shut in neighbouring district of Dindori. The local press reported panic as engineers took away pump handles without offering an explanation to villagers. In one village, Bichia, water was almost 13 times the safe limit.
It now seems incredible that so much poisoned water should have been tapped for drinking under a UN programme to provide safe water. The first instances of fluorosis in areas where underground water contained high fluoride levels were recorded in India 60 years ago. The government’s health ministry listed hot spots in several states where villagers suffered fluorosis from water in 1962. A task force to educate doctors and engineers was formed in 1986. Gourisankar Ghosh, who as head of India’s National Drinking Water Mission warned about the problem to little avail in the late 1980s, says: “There should have been far greater vigilance. We were sinking 60,000 boreholes a year and analysing water from at most a tenth of them.”
Since then geologists have devoted much time to plotting fluoride-bearing rocks. They have established that fluoride is associated with weathering granite rocks, and with water low in calcium. Gunnar Jacks of Sweden’s Royal Institute of Technology found that fluoride levels are highest in valley bottoms. Five years ago, he and geologists from the Central Ground Water Board of India recommended siting wells further up hillsides. Yet few doctors or water engineers in India seem to have heard of this.
Lack of communication is endemic, says Susheela of the fluorosis research foundation. “Engineers just presume that underground water is clean so they don’t test it. Doctors are not taught about fluorosis in our medical schools, so they don’t diagnose it.” What now? Digvijay Singh, Madhya Pradesh’s chief minister has announced plans to defluoridate water.
That was two years ago, and there’s still little sign of progress. In Hirapur, engineers have laid new water pipes but have not yet connected them to a new source. As a result, villagers have started to use an ancient open well, hauling buckets of water from a reservoir just as open to pollution from the surface. Many people now believe that water from the poisoned boreholes could have been used for washing, with the cleaner boreholes reserved for drinking water, says Raman. For its part, Unicef has backed efforts to treat water to remove fluoride as it is pumped to the surface. Early techniques were too expensive to sustain, and most defluoridation equipment installed over the past decade is out of action. Unicef is now testing a low-cost kit for homes.
Meanwhile, India’s escalating water crisis, which is forcing people to search for water deeper and deeper underground, is exacerbating the problem. “When you pump water from deeper underground, you are tapping older water, water which has been in contact with the rocks for longer. So it is more contaminated,” says Joshi. As the water tables continue to fall in response to demand, fluoride levels in thousands of boreholes, many of them still untested, will continue to rise.
SIDEBAR ARTICLE
When the village tap is contaminated
Tilaipani is like tens of thousands of Indian villages. Half a kilometre from the nearest road, and set in fields strewn with quartz stones, its economy runs on cattle, whose milk is sold in its main town, 12 kilometres away. But a few years ago, cattle drinking from new boreholes sunk by the department of public health engineering became crippled. Then the humans began to suffer, too.
It was here that Tapas Chakma, a young researcher, first uncovered the hidden epidemic of fluorosis across Mandla district. His studies, published last year in the journal Indian Paediatrics, found cases of severe knock knees in half of children under 20 years old in the village. In many cases the upper arm and the leg below the knee were splayed outwards.
The highest rate of deformity, 70 per cent, was among six to 10 year olds, who were toddlers when the new pumps first replaced surface wells. In the worst cases, he says, spines become entirely rigid and legs are so bowed inwards that they are permanently crossed.
Since 1996, all the handpumps in the village have been shut. A newly sunk borehole works only a few hours a day. As a result, women have resumed their age-old trek to fill buckets from a distant water hole. Have the victims been offered help? Some children receive a “scholarship grant” of 150 rupees a month (about £2) by way of compensation. No one knows if they’ll still get the money when they can’t get to school.
