It is now well established from clinical trials, animal studies, and in-vitro studies that fluoride exposure can weaken bone. The mechanisms by which fluoride exposure reduces bone strength are also well known. The matter that remains in controversy is the level of fluoride in drinking water that places society, or susceptible subsets of society, at risk for weakened bones and fracture. This page reviews the existing evidence.
Communities with 4 mg/L: Increased Risk of Fracture
The practice of fluoridating water supplies (0.7-1.2 mg/L) for the purpose of preventing tooth decay was launched in the 1950s on the basis that fluoride does not damage bone tissue at levels below 8 mg/L, or about 8 times more than the level of fluoride added to water. Since the 1980s, however, a number of studies have found that communities with 4 mg per liter of fluoride (the maximum fluoride level that is allowed in water) suffer elevated rates of bone fracture, including hip fracture. In 2006, the National Research Council (NRC) reviewed this research and concluded that the “weight of evidence” indicates that 4 mg/L increases the rate of fracture.
“The weight of evidence supports the conclusion that lifetime exposure to fluoride at drinking water concentrations of 4 mg/L and higher is likely to increase fracture rates in the population, compared with exposure to fluoride at 1 mg/L, particularly in some susceptible demographic groups that are prone to accumulating fluoride into their bones.” (NRC 2006, p. 165)
Communities with 2 mg/L: “Suggestive” Evidence of Risk
The NRC also considered studies investigating the fracture risk at fluoride levels below 4 mg/L. Although the NRC stated that it could make no “firm conclusions” about the fracture risk at these levels, it found the available evidence to be “suggestive” of an increased fracture risk between 1 mg/L and 4 mg/L. To quote:
“Overall, the committee finds that the available epidemiologic data for assessing bone fracture risk in relation to fluoride exposure around 2 mg/L is suggestive but inadequate for drawing firm conclusions about the risk or safety of exposures at that concentration.” (NRC 2006, p. 170).
The “suggestive” evidence noted by the NRC includes a Finnish study (Kurttio 1999), a Chinese study (Li 2001), and a Mexican study (Alarcon-Herrera 2001), the combined findings of which “lend support to gradients of exposure and fracture risk between 1 and 4 mg/L.” (NRC, p. 164).
Communities with 1 mg/L: Mixed Evidence of Fracture Risk
A number of studies have sought to determine whether fluoridated drinking water (1 mg/L) also increases the risk of bone fracture. The results of these studies have been mixed, with some studies finding increases in bone fracture, other studies finding no effect, and others finding reductions in fracture risk. As noted by scientists on both sides of the fluoride debate, however, the usefulness of studies comparing overall fracture rates in fluoridated vs. non-fluoridated communities is limited. Most of the studies, for example, only examined older populations that had no exposure to fluoridated water during their childhood (the period of life when fluoride uptake into bone is at its highest point). In fact, most of the studies on the fracture risk from fluoridated water have involved adult populations with less than 20 years of exposure to fluoridated water. By contrast, the studies dealing with the effect of higher fluoride levels 2 to 4 mg/l dealt with populations that had lifetime exposures to the water. The available epidemiological evidence on fluoridation and fracture thus provide little guidance, therefore, about the impact of lifetime exposures to artificially fluoridated water.
A Narrow Margin of Safety
Although current epidemiological evidence fails to demonstrate a detectable population-wide fracture risk from consuming fluoridated water, the evidence of an increasing fracture risk between 1 and 4 mg/l indicates that there is a very narrow margin of safety between the level of fluoride that does, and does not, increase the risk of fracture. This becomes particularly evident when comparing the doses that people receive in fluoridated areas with the doses that the epidemiological studies have associated with increased fracture risk. The following figure displays the daily fluoride doses associated with an increased risk of hip fracture in the Li (2001) study:
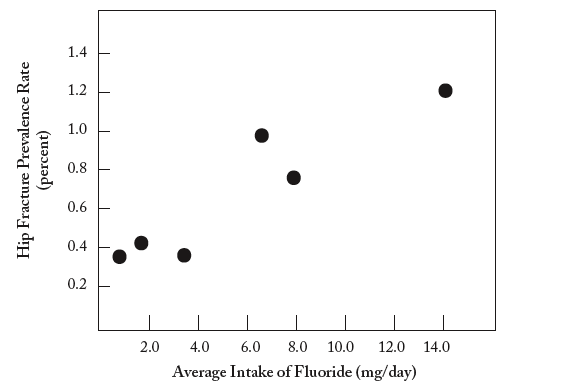
Data from: Li Y, et al. (2001). Effect of long-term exposure to fluoride in drinking water on risks of bone fractures. Journal of Bone and Mineral Research 16:932-9.
As can be seen, the risk of hip fracture is distinctly elevated in communities with an average dose of 6 to 8 mg per day. To put this dose into perspective, the U.S. Department of Health and Human Services has estimated that adults living in fluoridated communities ingest between 1.6 and 6.6 mg of fluoride per day. (DHHS 1991). This dose range overlaps the dose range associated with hip fracture risk.
Such a narrow margin of safety is particularly problematic when considering that some subsets of the population, including those with advanced kidney disease, are particularly vulnerable to fluoride’s toxic effects, and can be affected at doses well below those that cause harm in others.
Recently Published Evidence
The last study investigating the bone fracture risk in fluoridated communities was published in 2000. (Phipps 2000). Since that time, several studies have been published which add to the weight of evidence that fluoridated water can damage bone. Unlike the epidemiological studies on fracture rates, the new research has used methods which allow the risk of fluoride to be assessed based on the individual’s actual exposure, not merely the fluoride level in their water supply.
- Ng (2004): This study assessed the relationship between bone fluoride content and various parameters of bone quality in dialysis patients with renal osteodystrophy living in the fluoridated city of Toronto, Canada. It found that the fluoride content of bone significantly correlated with the degree of osteomalacia, a bone-softening disease that is marked by excessive accumulation of osteoid (unmineralized tissue). One of the well-known effects of osteomalacia is bone fracture. Previous studies, from both New Jersey and Finland, have reported similar findings. (Alhava 1985; Stein & Granik 1980)
- Levy (2009): This study assessed the relationship between total daily fluoride intake during the first 11 years of life and bone density in both boys and girls. Although the authors go out of their way to downplay the significance of their results, their data shows that girls with the highest fluoride intake consistently had less bone mineral in their skeleton. Although the differences were not always statistically significant, the trend in the data is pretty notable and indicates that fluoride’s detrimental effect on cortical bone can occur at doses ingested by children in the general population. If confirmed, this result highlights the problem, mentioned above, of relying on epidemiological studies of fracture risk in populations that were not exposed to fluoridated water from birth.
References:
4 mg/L: Increased Hip and Other Fractures
“The purpose of this study was to determine the prevalence of bone fracture, including hip fracture, in six Chinese populations with water fluoride concentrations ranging from 0.25 to 7.97 parts per million (ppm). . . . It is concluded that long-term fluoride exposure from drinking water containing > or =4.32 ppm increases the risk of overall fractures as well as hip fractures.
SOURCE: Li Y, et al. (2001). Effect of long-term exposure to fluoride in drinking water on risks of bone fractures. Journal of Bone and Mineral Research 16:932-9.
“[A] study of bone mass and fractures was begun in 827 women aged 20-80 years in three rural Iowa communities selected for the fluoride and calcium content of their community water supplies . . . Residence in the higher-fluoride (4 ppm) community was associated with a significantly lower radial bone mass in premenopausal and postmenopausal women, an increased rate of radial bone mass loss in premenopausal women, and significantly more fractures among postmenopausal women.”
SOURCE: Sowers MR, et al. (1991). A prospective study of bone mineral content and fracture in communities with differential fluoride exposure. American Journal of Epidemiology 133: 649-660.
1 mg/L: Increased Hip Fracture
“This study examines the geographic distribution of hip fracture incidence in the United States at the county level. To this end, data are obtained from the Health Care Financing Administration (HCFA) and the Department of Veteran Affairs that identify all hospital discharges with a diagnosis of hip fracture for women aged 65 years and older for the period 1984 through 1987…After exclusions, 541,985 cases remained eligible for study… There is a weak positive association between the percent of county residents who receive fluoridated water and hip fracture incidence in the unadjusted analysis that is strengthened after adjustment.”
SOURCE: Jacobsen SJ, et al. (1990). Regional variation in the incidence of hip fracture: US white women aged 65 years and olders. Journal of the American Medical Association 264(4): 500-2.
“We found a significant positive correlation between fluoride levels and discharge rates for hip fracture. This relationship persisted for both women and men… Using an appropriately weighted regression model, there appears to be a positive ecologic association between fluoride levels of county water supplies and fracture discharge rates. This ecologic association is consistent with a recently published study and others currently in progress.”
SOURCE: Cooper C, et al. (1991). Water fluoridation and hip fracture. Journal of the American Medical Association 266: 513-514.
” An ecologic study compared fracture rates in 216 counties with natural fluoride levels greater than 0.7 ppm with rates in 95 counties with naturally low fluoride (less than 0.4 PPM) in the drinking water. In general, with increasing dose of fluoride in the drinking water the hip fracture ratio also increased.”
SOURCE: Keller C. (1991) Fluorides in drinking water. Unpublished results. In: Gordon SL, Corbin SB. (1992) Summary of Workshop on Drinking Water Fluoride Influence on Hip Fracture on Bone Health. Osteoporosis International 2: 109-117.
“The incidence of femoral neck fractures in patients 65 years of age or older was compared in three communities in Utah, one with and two without water fluoridated to 1 ppm. . . . We found a small but significant increase in the risk of hip fracture in both men and women exposed to artificial fluoridation at 1 ppm, suggesting that low levels of fluoride may increase the risk of hip fracture in the elderly.”
SOURCE: Danielson C, et al. (1992). Hip fractures and fluoridation in Utah’s elderly population. Journal of the American Medical Association 268: 746-748.
“In order to assess the association between water fluoridation and hip fracture, we identified 129 counties across the United States considered to be exposed to public water fluoridation and 194 counties without exposure. . . There was a small statistically significant positive association between fracture rates and fluoridation. The relative risk (95% confidence interval) of fracture in fluoridated counties compared to nonfluoridated counties was 1.08 (1.06 to 1.10) for women and 1.17 (1.13 to 1.22) for men.”
SOURCE: Jacobsen SJ, et al. (1992). The association between water fluoridation and hip fracture among white women and men aged 65 years and older; a national ecologic study. Annals of Epidemiology 2: 617-626.
“The 1985 Fluoridation Census data were used for the 438 counties with populations over 100,000, which represents about 70% of the US population. . . . The percentage of the population that received natural or adjusted fluoride (approximately 1 ppm) was estimated for each county. Medicare data for 1984-1987 were used to calculate the annual incidence of age adjusted hip fractures for white males and females age 65 and older. As the percentage of individuals exposed to fluoridated water increased within a county, the hip fracture rate generally rose for both sexes, but not in a smooth linear fashion… Adjustment for county latitude and longitude produced higher correlation values and significance for females and males.”
SOURCE: May DS, Wilson MG. (1992). Hip fractures in relation to water fluoridation: an ecologic analysis. Unpublished Results: In Gordon SL, Corbin SB. (1992). Summary of Workshop on Drinking Water Fluoride Inflruence on Hip Fracture on Bone Health. Osteoporosis International 2:109-117.
“The purpose of this study was to compare hip fracture hospitalization rates between a fluoridated and a non-fluoridated community in Alberta, Canada . . . . No statistically significant difference was observed in the overall rate, and only minor differences were observed within age and sex subgroups . . . . [A]lthough a statistically significant increase in the risk of hip fracture was observed among Edmonton men, this increase was relatively small (RR=1.12).”
SOURCE: Suarez-Almazor M, et al. (1993). The fluoridation of drinking water and hip fracture hospitalization rates in two Canadian communities. American Journal of Public Health 83: 689-693.
“In the retrospective cohort study based on record linkage, the authors studied a cohort of persons born in 1900-1930 (n = 144,627), who had lived in the same rural location at least from 1967 to 1980. Estimates for fluoride concentrations (median, 0.1 mg/liter; maximum, 2.4 mg/liter) in well water in each member of the cohort were obtained . . . . No association was observed between hip fractures and estimated fluoride concentration in the well water in either men or women when all age groups were analyzed together. However, the association was modified by age and sex so that among younger women, those aged 50-64 years, higher fluoride levels increased the risk of hip fractures. Among older men and women and younger men, no consistent association was seen. The adjusted rate ratio was 2.09 (95% confidence interval: 1.16, 3.76) for younger women who were the most exposed (>1.5 mg/liter) when compared with those who were the least exposed (< or =0.1 mg/liter). The results suggest that fluoride increases the risk of hip fractures only among women.”
SOURCE: Kurttio PN, et al. (1999). Exposure to natural fluoride in well water and hip fracture: A cohort analysis in Finland. American Journal of Epidemiology 150: 817-824.
“Hip fractures and knee DJD joint replacements among those >65 years for 1991-1996 were compared between one community with and two without fluoridated water. . . . The only age-adjusted rate achieving statistical significance was the age-specific rate for hip fracture among women 75-84 years, with a RR = 1.43 (95% CI, 1.02-1.84). The rate of hip fracture among women aged 85+ approached significance with a RR = 1.42 (CI, 0.98-1.87). The hip fracture rate among women aged 65-74, however, showed no association and caused the age-adjusted RR to be non-significant.”
SOURCE: Hegmann KT, et al. (2000). The effects of fluoridation on degenerative joint disease (DJD) and hip fractures. American Journal of Epidemiology S18.
1 mg/L: No Effect on Hip Fracture, Increased Wrist Fracture
“The purpose of this study was to examine whether geographic area or water fluoride were related to the occurrence of fractures among the elderly in the United States. We used a 5% sample of the white U.S. Medicare population, aged 65 to 89 years during the period 1986-1990, to identify fractures of the hip, proximal humerus, distal forearm, and ankle. The association of geographic region and fluoridation status with fracture rates was assessed using Poisson regression. We found that rates of hip fracture were generally lower in the northern regions of the United States and higher in the southern regions. For fractures of the distal forearm and proximal humerus, lower rates were found in the Western states, and higher rates in the East. No discernible geographic pattern was found for ankle fractures. Adjustment for water fluoridation did not influence these results. Independent of geographic effects, men in fluoridated areas had modestly higher rates of fractures of the distal forearm and proximal humerus than did men in nonfluoridated areas; no such differences were observed among women, nor for fractures of the hip or ankle among either men or women. In conclusion, our data suggest that fractures of the distal forearm and proximal humerus have etiologic determinants distinct from those of fractures of the hip or ankle.”
SOURCE: Karagas MR, et al. (1996). Patterns of Fracture among the United States Elderly: Geographic and Fluoride Effects. Ann. Epidemiol. 6 (3): 209-216.
1 mg/L: Decreased Hip Fracture, Increased Wrist Fracture
“Outcomes were compared in women with continuous exposure to fluoridated water for the past 20 years (n=3218) and women with no exposure during the past 20 years (n=2563). . . . In women with continuous exposure the multivariable adjusted risk of hip fracture was slightly reduced (risk ratio 0.69, 95% confidence interval 0.50 to 0.96, P=0.028) as was the risk of vertebral fracture (0.73, 0.55 to 0.97, P=0.033). There was a non-significant trend toward an increased risk of wrist fracture (1.32, 1.00 to 1.71, P=0.051) . . . .”
SOURCE: Phipps KR, et al. (2000). Community water fluoridation, bone mineral density and fractures: prospective study of effects in older women. British Medical Journal. 321: 860-4.
“The relation between fluoride intake and risk of osteoporotic fractures remains unclear. The lack of individual measures of long-term fluoride intake has limited epidemiologic studies. We used toenail fluoride in this study as a measure of long-term intake to evaluate the relation between fluoride intake and subsequent risk of hip and distal forearm fractures. . . . [I]ncreasing levels of toenail fluoride have a slight protective on the risk of hip fractures but are associated with a more marked rise in risk of forearm fractures.”
SOURCE: Feskanich D, et al. (1998). Use of toenail fluoride levels as an indicator for the risk of hip and forearm fractures in women. Epidemiology 9(4): 412-6.
1 mg/L: No Effect on Hip Fracture
The following studies did not find any association between water fluoridation (~1 mg/L) and hip fracture:
Hillier S, et al. (2000). Fluoride in drinking water and risk of hip fracture in the UK: a case control study. The Lancet 335: 265-2690.
Lehmann R, et al. (1998). Drinking Water Fluoridation: Bone Mineral Density and Hip Fracture Incidence. Bone. 22: 273-278.
Jacqmin-Gadda H, et al. (1998). Risk factors for fractures in the elderly. Epidemiology 9: 417-423.
Cauley J. et al. (1995). Effects of fluoridated drinking water on bone mass and fractures: the study of osteoporotic fractures. J Bone Min Res 10(7): 1076-86.
Jacobsen SJ, et al. (1993). Hip Fracture Incidence Before and After the Fluoridation of the Public Water Supply, Rochester, Minnesota. American Journal of Public Health. 83: 743-745.
Arnala I, et al. (1986). Hip fracture incidence not affected by fluoridation. Osteofluorosis studied in Finland. Acta Orthop Scand. 57: 344-348.
Madans J, et al. (1983). The relationship between hip fracture and water fluoridation: an analysis of national data. Am J Public Health 73: 296-298.
