Abstract
Child dental caries (i.e., cavities) are a major preventable health problem in most high-income countries. The aim of this study was to compare the extent of inequalities in child dental caries across four high-income countries alongside their child oral health policies. Coordinated analyses of data were conducted across four prospective population-based birth cohorts (Australia, n = 4085, born 2004; Québec, Canada, n = 1253, born 1997; Rotterdam, the Netherlands, n = 6690, born 2002; Southeast Sweden, n = 7445, born 1997), which enabled a high degree of harmonization. Risk ratios (adjusted) and slope indexes of inequality were estimated to quantify social gradients in child dental caries according to maternal education and household income. Children in the least advantaged quintile for income were at greater risk of caries, compared to the most advantaged quintile: Australia: AdjRR = 1.18, 95%CI = 1.04–1.34; Québec: AdjRR = 1.69, 95%CI = 1.36–2.10; Rotterdam: AdjRR = 1.67, 95%CI = 1.36–2.04; Southeast Sweden: AdjRR = 1.37, 95%CI = 1.10–1.71). There was a higher risk of caries for children of mothers with the lowest level of education, compared to the highest: Australia: AdjRR = 1.18, 95%CI = 1.01–1.38; Southeast Sweden: AdjRR = 2.31, 95%CI = 1.81–2.96; Rotterdam: AdjRR = 1.98, 95%CI = 1.71–2.30; Québec: AdjRR = 1.16, 95%CI = 0.98–1.37. The extent of inequalities varied in line with jurisdictional policies for provision of child oral health services and preventive public health measures. Clear gradients of social inequalities in child dental caries are evident in high-income countries. Policy related mechanisms may contribute to the differences in the extent of these inequalities. Lesser gradients in settings with combinations of universal dental coverage and/or fluoridation suggest these provisions may ameliorate inequalities through additional benefits for socio-economically disadvantaged groups of children.
Full Text:
Introduction
Despite great improvements in the oral health of populations, dental caries (an infectious disease caused by certain types of bacteria [1]) remains a significant and preventable population health problem even in high-income countries [2, 3], and particularly for children [4]. This is highlighted by the recent WHO call for a global oral health strategy by 2022 involving major systems reforms placing equity and social justice at the core [5]. Dental caries is the most common disease of childhood [6] and affects up to 60–90% of school-aged children in most high-income countries [7–9]. Nearly 486 million children worldwide suffer from caries of primary teeth, posing a major global public health challenge [10].
Poor oral health can negatively impact the quality of life of children into adulthood. Major risk factors contributing to dental caries and its complications are the limited availability and accessibility of oral health services, poor oral hygiene behaviors (including inadequate tooth brushing, lack of flossing), adverse living conditions, and unhealthy lifestyles (including dietary patterns) [7, 11]. For example, frequent, excessive consumption of sugary food and beverages is thought to be a major cause of dental caries [7]. Poor oral health can impair a child’s ability to eat, sleep, and socialize, which may result in ongoing adverse outcomes [1, 6, 12, 13]. These outcomes can include pain, high economic costs, poor nutrition, and impaired growth due to painful symptoms, school absenteeism, and lower quality of life [1, 14]. The health burden of dental caries is under-recognized, and socio-economically disadvantaged populations are disproportionately affected [15].
Children from low-income countries have a greater risk of caries and higher unmet treatment needs than those living in high-income countries [8]. The Global Burden of Disease 2017 study [2] showed that social inequalities exist in the distribution of oral health conditions such as dental caries. In 2017, the estimated prevalence of current dental decay (excluding missing or filled teeth) in deciduous teeth was 7.8% (532 million cases). While this burden lies primarily within low-income countries (265 million cases) a significant burden has been observed within high-income countries (41 million cases) [2]. Overall, the number of cases with current dental decay in deciduous teeth decreased in high-income countries between 1990 and 2017, while for low-income countries it has increased [2]. While the prevalence of dental caries in primary and permanent teeth varies for children in different continents [16], the overall high international prevalence calls for implementation of appropriate strategies to improve oral health and close equity gaps.
Poor oral health has a growing impact on vulnerable and marginalized populations of children. Families who are disadvantaged by low income and/or low education experience higher levels of dental caries, across both high-income and low-income countries [7, 17–20]. International reviews highlight the multifactorial aetiology of dental caries underpinned by the social determinants of health, but modulated by biological, social, economic, cultural, and environmental factors [21]. Recommended approaches to reduce prevalence include interventions that begin in the first year of life; evidence and risk-based management; and health care system financing that ensures the accessibility of preventive care [22].
The delivery of health promotion strategies including implementation of free dental care coverage for all children combined with public health measures, such as water fluoridation, have led to meaningful reductions in dental caries and social inequalities [21, 23–25]. Although the effectiveness of water fluoridation has been contested, in Australia water fluoridation is associated with reduced experience of caries, benefitting all socio-economic strata of the community [23]. International estimates suggest that water fluoridation reduces tooth decay by at least 25% in children and adolescents [24, 26], and that tooth decay in adults may be prevented by providing access to fluoridated water from an early age [24].
Child dental caries remains a significant and preventable chronic public health disease in high-income countries [27], with clear social inequalities and long term impacts on quality of life. International studies comparing cohorts from high-income countries with diverse health and social policies can facilitate our understanding of how variation in policy across jurisdictions impacts dental caries. Elucidating Pathways of Child Health Inequalities (EPOCH) is an international research project that aims to address knowledge gaps underlying childhood health disparities [28]. The EPOCH study, funded by the Canadian Institutes of Health Research (CIHR), was conceived and planned by researchers in the International Network for Research on Inequalities in Child Health (INRICH) [www.inrichnetwork.org]. This study utilized harmonized data from the EPOCH research project; specifically, four large, population-representative birth cohort studies in high-income countries with variable forms of universal health insurance and oral health policy: Australia, Québec (Canada), Rotterdam (the Netherlands), and Southeast Sweden (see S1 Table).
Comparisons across these high-income jurisdictions/countries can provide rich insight into child dental caries prevalence, and associated health policies and social inequalities. This research is both timely and necessary to advance potential future policy action. The aim of the current study was to investigate comparative social gradients and associated risk factors for child dental caries using longitudinal cohort data across four high-income countries. Observing differential childhood caries outcomes according to household income and maternal education would provide evidence to determine whether childhood dental caries was experienced equitably within high-income countries. Policy mechanisms that could explain any differences in the extent of inequalities, such as oral health care provision and water fluoridation, were then considered.
Materials and methods
Data sources
The EPOCH Collaborative Group investigates inequalities across a diversity of health outcomes up to age 10 years by comparing birth cohorts from high-income countries with diverse social policies. Coordinated analyses of health inequalities are being conducted across this series of cohorts using identical statistical methods and comparable variables. Analyses are underpinned by processes of harmonization to enable meaningful comparative interpretation of social gradients according to maternal income and education [28]. Concordia University Human Research Ethics Committee certified the ethical acceptability for EPOCH’s secondary data use (#2011028). All original birth cohorts complied with the ethical standards of their relevant institutional and/or national committees and with the Helsinki Declaration of 1964, and its later amendments. Information summarizing what participation would involve was provided in both oral and written form.
For this study, data were drawn from four longitudinal cohorts within EPOCH, each including measures of dental caries: the national Longitudinal Study of Australian Children–Birth cohort (LSAC–B cohort) in Australia; and three regional studies: Québec Longitudinal Study of Child Development (QLSCD) in Québec, Canada; The Generation R Study in Rotterdam, the Netherlands; and, Alla Barn i Sydöstra Sverige (ABIS; English translation: All Babies in Southeast Sweden) in Southeast Sweden. Each study recruited women and children during pregnancy or infancy and prospectively followed up families. Further description of the cohort design, participants, survey weighting methods, ethics approvals and measures are provided in Table 1. All cohorts selected for inclusion included pertinent details regarding the nature/administration and timing of dental caries measures or assessments, albeit study methods differed (e.g., caregiver report vs. dental exam photographs). Further, harmonization of these dental outcomes as well as coordinated analyses and harmonization of income and education classifications increased confidence that findings reflect robust jurisdictional differences. Measures included in this synthesis and the timing of administration are detailed as follows.

Table 1. Cohort descriptions and variable definitions. https://doi.org/10.1371/journal.pone.0268899.t001
Measures
Outcome measure: Child dental caries.
Dental caries (yes/no) was measured across cohorts. In Australia (at age 8–9 years), Québec (at age 8–9 years), and Southeast Sweden (at age 5 years), the primary caregiver was asked to report on their child’s history of dental caries including extractions and fillings within the study interview, while in Rotterdam (at age 6 years), direct observation of intraoral photographs was used. For each cohort, binary categories (yes/no) of dental caries were classified.
Socio-economic position (SEP).
In line with the EPOCH foundational work undertaken to determine internationally comparable measures [28], maternal education level and household income were considered as indicators of socio-economic position, reflecting their wide applicability in epidemiological research, availability and comparability across cohorts. Maternal education was measured at baseline across all four cohorts; household income was measured within early childhood (Australia: at baseline (0–1 years); Québec: at baseline (0–1 years); Rotterdam: at age 6 years; and Southeast Sweden: at age 1–3 years). For each cohort, low/middle/high categories of maternal education were classified to provide comparative definitions across education systems. Low maternal education typically reflected low or incomplete secondary education; middle reflected completed secondary education, technical or vocational qualifications; and high reflected a university degree or higher (see Table 1 for full details).
Household income quintiles were classified within the participating cohorts, in Québec using gross income before tax (additionally adjusting regression models for household size); and in the other three cohorts using net income after tax and transfers had been accounted for.
Oral health risk factors.
Children’s consumption of sugary food and sugary drinks (classified within the cohorts as less than daily/once a day/more than once a day) were measured across cohorts (at ages 8–9 years in Australia, 10 years in Québec, 6 years in Rotterdam, and 5 years in Southeast Sweden). Jurisdictions varied in whether and how tooth brushing was measured, so it was not included due to being unable to derive a consistent indicator. Ideally, whether oral health services were provided for preventive care would have also been included. It was also unable to be ascertained whether families sought care for preventive reasons or in response to caries experienced by the child. Oral health service provision was thus explored at a policy level by jurisdiction. Similarly, naturally occurring water fluoride and policies for fluoridation were explored at the jurisdiction level.
Demographic variables.
For each cohort, children’s age and sex (classified as male/female) were recorded, along with geographic area (city or urban/rural or remote).
Statistical analysis
Child dental caries by cohort.
Rates of the child having ever experienced dental caries by the applicable age at follow up were estimated for each of the cohorts.
Within cohort social gradients.
Relative risk ratios were estimated to quantify the association between maternal education, income, and childhood dental caries. These estimates were adjusted to account for: sex, geographic area, and sugary food and drink consumption (as available for each cohort). Risk ratios were estimated within each population using a generalized linear model with log link function and robust variance estimation [41].
The Slope Index of Inequality (SII) was estimated for each cohort, representing the absolute difference in caries prevalence that would be expected between children in the most and least advantaged households (according to income and maternal education respectively) [42]. The SII is a regression-based index estimating the magnitude of inequalities in health. Differences between the least and the most advantaged groups were estimated for each cohort using linear regression of the weighted prevalence estimates for each of the income quintiles/three levels of maternal education with the mid points of the cumulative fractions of the socio-economic groups as the predictors.
Australian and Southeast Sweden data were analyzed using Stata version 15. Québec data were analyzed using SPSS version 25. Rotterdam data were analyzed using R version 3.6.1.
Policy and service context.
The oral health care policy and service systems were described for each jurisdiction to detail local contexts, noting public funding, out of pocket expenses, access to dental services, and water fluoridation policies (S1 Table).
Results
Cohort characteristics
Cohort characteristics such as participant retention rates are detailed in Table 1. Cohorts had a similar balance of males and females (Table 2). The Rotterdam cohort recruited an urban population, while the other three cohorts included both urban and non-urban families at recruitment (during pregnancy or infancy).

Table 2. Participant details for each cohort. https://doi.org/10.1371/journal.pone.0268899.t002
Child dental caries.
By age 8/9 years, over half (55%) of Québec children had experienced caries (parent-reported untreated cavities, treated cavities and extracted teeth; Table 2). In Australia, the percentage of children with caries was 41% by age 8/9 years (parent-reported decayed, missing, or filled teeth). In Rotterdam, dental caries by age 6 years were identified for 25% of children (intraoral photographs to assess decayed, missing or filled teeth due to cavities) but 20% of the children were not assessed, so the prevalence might be higher (31.5% amongst children assessed). In Southeast Sweden, caries were lowest at 12% for children aged 5 years (parent-reported cavities). Direct comparisons of prevalence are cautioned given differences in age and assessment of caries.
Risks for child dental caries within each jurisdiction
Inequalities by income and maternal education.
Fig 1 illustrates adjusted risk ratios examining association between income, maternal education and caries for each cohort. Adjusted risk ratios for Australia (AdjRR = 1.18, 95%CI = 1.01–1.38), Southeast Sweden (AdjRR = 2.31, 95%CI = 1.81–2.96), Rotterdam (AdjRR = 1.98, 95%CI = 1.71–2.30), and Québec (AdjRR = 1.16, 95%CI = 0.98–1.37) indicate higher risk of caries for children of mothers with the lowest level of education (Table 3).
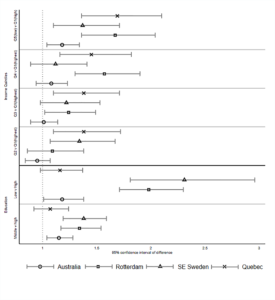
Fig 1. Forest plots illustrating inequalities in child dental caries by income and maternal education. https://doi.org/10.1371/journal.pone.0268899.g001
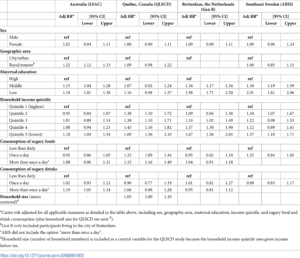
Table 3. Adjusted risk ratios for child dental caries. https://doi.org/10.1371/journal.pone.0268899.t003
Examining income, those in the least advantaged quintile were at greater risk of caries for all cohorts (compared to the most advantaged quintile: Australia: AdjRR = 1.18, 95%CI = 1.04–1.34; Québec: AdjRR = 1.69, 95%CI = 1.36–2.10; Rotterdam: AdjRR = 1.67, 95%CI = 1.36–2.04; Southeast Sweden: AdjRR = 1.37, 95%CI = 1.10–1.71). Income gradients within Rotterdam and Québec reflected higher risk according to each quintile of disadvantage.
Oral health risk factors.
Consumption of sugary drinks or foods varied substantially across the four cohorts (Table 2). Accordingly the associations with dental caries also varied (Table 3). In Australia, child dental caries was associated with high sugary beverage consumption (more than once a day vs less than daily, AdjRR = 1.19, 95%CI = 1.05–1.34). In Québec, child dental caries was associated with sugary food consumption (once a day, AdjRR = 1.25, 95%CI = 1.09–1.44; more than once a day AdjRR = 1.32, 95%CI = 1.16–1.49). In Rotterdam and Southeast Sweden, there was little evidence to suggest that consumption of sugary foods or drinks was associated with child dental caries.
Geographic risk factors.
In Australia, child dental caries was associated with living in rural or remote areas compared to urban areas (AdjRR = 1.22, 95%CI = 1.12–1.33). Differences in caries risk according to geographic area were less evident for children in Québec and Southeast Sweden (children in Rotterdam were all living in urban areas at birth).
Slope Index of Inequality (SII)
SII by maternal education and income are illustrated for each cohort in Fig 2. For maternal education, the strongest gradient was in Rotterdam (SII = -45), estimating a 45% difference in caries prevalence when comparing the children whose mothers had the lowest level of education to the highest. Shallower gradients for Québec, Southeast Sweden, and Australia (SII = -30, -16, -15, respectively) reflected less difference in prevalence of child dental caries according to maternal education. For income quintiles, the gradients for Québec and Rotterdam were similar (-36 and -34); Australia had a shallower gradient (-16); while the Southeast Sweden line was close to flat (-2). The SII estimates absolute unadjusted differences with the interpretation that, in the absence of confounding, if all families were as wealthy as the richest family, the prevalence of caries would be 2% lower for Southeast Sweden, 16% lower for Australia, 34% lower for Rotterdam, and 36% lower for Québec.
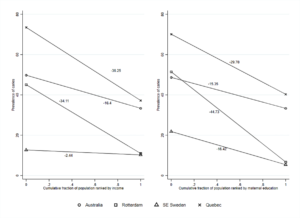
Fig 2. Slope Index of Inequality (SII) in child dental caries by income and education. https://doi.org/10.1371/journal.pone.0268899.g002
Discussion
The health burden of child dental caries within high-income countries is under-recognized and preventable, disproportionately affecting socio-economically disadvantaged families. This study aimed to develop policy-relevant evidence, specifically targeting inequalities, through the comparison of rates of child dental caries and the extent of inequalities across high-income countries (Australia, Québec (Canada), Rotterdam (the Netherlands), and Southeast Sweden). Using data from large, representative birth cohorts, this study found variability in prevalence and distribution of child dental inequalities across these jurisdictions. Overall, the identified prevalence of caries varied from 12% to 55% of the population, noting the differences in ages (i.e., 8–9 years for Québec versus 5 years for Southeast Sweden).
In all countries, the current study found that children living in families with lower maternal education or household income were more likely to experience dental caries. Southeast Sweden and Rotterdam had greater inequality related to maternal education than Australia and Québec. Inequalities according to income were greatest in Québec and Rotterdam. Taking into account underlying population income distribution, the SII for Rotterdam and Québec were similarly steep (-34 and -36), than Australia’s more moderate SII (-16). The SII for Southeast Sweden was close to flat (-2), which may reflect the social system with transfer of money to families with low income, in combination with completely free childhood dental care (including preventive care) and natural fluoridation of the drinking water. In contrast, the Netherlands similarly has free dental care but the gradient was still evident. These estimates suggest potential absolute reductions in dental caries of between 2% and 36% if inequalities were ameliorated and all children held the same advantage as the richest families in each jurisdiction.
Findings from the present study were consistent with previous research demonstrating social inequalities in child dental caries within high-income countries. In Australia (also using the LSAC cohort), the odds of having dental caries were highest for children living in families with low socio-economic position (SEP: a composite of family income, education and occupation), and in areas with non-fluoridated water supply [43]. Low maternal education has also been shown to be associated with child dental caries in a longitudinal study of Indigenous Australian children [44]. In the Netherlands (also using the Generation R cohort), low maternal education was associated with higher odds of dental caries [18]. In Sweden, low maternal education and low family income were associated with higher rates of child dental caries [45].
The different levels of inequality in dental caries across the cohorts are likely to reflect substantive differences in child oral health policy across jurisdictions. Drawing on the oral health and service policies detailed in S1 Table, one potential reason may be due in part to the protective effect of water fluoridation. Australian research has shown that fluoridation of the water supply may have a beneficial impact in preventing dental caries, to some extent ameliorating the social gradient [24, 43]. This evidence is limited, with a Cochrane review reporting insufficient evidence to support this claim due to the general absence of causal evidence [46]. Australia mostly has very low levels of naturally occurring fluoride; yet, community water fluoridation means that around 89% of Australians have access to fluoridated drinking water [24]. Sweden’s drinking water only contains a natural variation of fluoride; however, fluoride levels do vary within municipalities [47]. While the current study was unable to ascertain this relationship, it is plausible that the artificially fluoridated drinking water in Australia and natural fluoridation in Sweden contributes to the lower levels of inequality demonstrated in these two countries. Previous Australian research has shown that fluoridation of the water supply seems to ameliorate (although not eliminate) inequalities [43]. In Québec, fluoridation of water is not widespread; less than 3% of the population has access to fluoridated water [48]. This has been identified as one likely reason why dental caries is far more prevalent than in neighboring provinces like Ontario (over 70% fluoridated water) [49]. In the Netherlands, fluoride is not added to the drinking water; the natural concentration of fluoride varies between 0.05 and 0.25 mg/L.
Further differences for socio-economically disadvantaged families may relate to the inclusion of dental care in universal health coverage. Universal coverage reduces barriers to care which addresses caries through prevention and prompt treatment [2]. In the current study there was evidence of considerable variability in oral health services (S1 Table). For example, in Australia and Québec, the publicly funded health system provides limited oral health coverage, potentially resulting in large out of pocket expenses. In Québec, children aged under 10 years have access to free dental services, but their parents do not have this coverage, which may impede service use [50]. In the Netherlands, the costs for basic dental care for children (until 18 years) are reimbursed via the obligatory (by law) ‘basic health insurance’ [18]. In Sweden, however, oral health is free of charge from birth to 23 years of age with an expectation and encouragement for preventive dental care.
Strengths and limitations
A major strength of the current study was the data from four large, population representative cohort studies which enabled comparisons from jurisdictions providing rich, valuable information on child dental caries and social inequalities. However, this synthesis also posed some challenges, as the independent cohorts were not designed together. Some measures, such as maternal education, were captured in nearly identical ways and at similar time-points across all four cohorts. Others, such as child dental caries, were measured using different assessment methods at different ages across cohorts (see Table 1 for more detail).
In Australia, Québec, and Southeast Sweden, child dental caries was measured using parent-report within the survey interview, while the Rotterdam cohort used direct observation of intraoral photographs. Validation of parent-reported single-item indicators of child dental caries has recognized their potential underestimation of dental caries [51]. Using dental clinical examinations or dental records to validate parent-reported dental caries would be ideal in future studies [17]. Different criteria for identifying child dental caries means that caution should be held in interpreting differences in prevalence between jurisdictions [22]. However, the coordinated analysis enabled a high degree of harmonization, increasing confidence that findings reflect actual population differences.
Policy modifiable oral health factors, such as water fluoride level and use of dental services, are known to impact inequalities in rates of child dental caries in Australia [43]. However, data were not available to examine these relationships internationally. Future research could endeavor to examine the role of these factors on inequalities in rates of child dental caries across countries.
Finally, each cohort has its own limitations that should be recognized including population groups for whom the current findings may not apply. In the Australian cohort, children from very remote areas and Aboriginal and Torres Strait Islander children were not well represented and care should be taken in extrapolating findings [52]. In the Québec cohort, children born in the Nord-du-Québec, Terres-Cries-de-la-Baie-James, Nunavik, or other Indian Reserves, about 2.1% of the population, were excluded [33]. The Rotterdam cohort included an urban population of children with multi-ethnic composition (68% Dutch/Western, 32% Non-Western ethnic background), for whom socio-economic disadvantage may be inequitably linked to relatively lower levels of health literacy and less favourable health behaviours [18].
Public health implications
The current study findings align and provide further empirical evidence supporting recent recommendations from the WHO global strategy for oral health [5]. Key elements of this strategy (summarized in S2 Table) include the need for major system reforms to provide inclusive, accessible, and affordable oral health-care including the need to close financing gaps to align goals of universal primary health care coverage, and to establish data-driven evidence-informed policy for oral health (including the importance of tackling risk factors such as sugar consumption) and health care. While the WHO recommendations primarily focus on low- and middle-income countries, the current study is both timely and necessary to advance potential policy action towards equitable oral health and provision of care within high-income jurisdictions [5].
Inequalities in dental caries requires a broad public health approach that simultaneously focuses on the social determinants of health while more specifically considering population wide oral health and health care system solutions. Health care systems that offer and encourage free regular dental check-ups for all children and teenagers in public or private dental care are beneficial for public health. For example, in Southeast Sweden, the combination of universally available dental care (including for prevention), naturally fluoridated water, and low consumption of sugar seem to have resulted in a lower prevalence of dental caries for children. This suggests the combination of strategies that may be necessary to ameliorate the social gradient in childhood caries.
Similarly, it must be noted that fluoridated water is not available to all children in the four countries included in this study, despite its biologically demonstrated protective effects (and no demonstrated significant harm [23, 46]). Continued promotion of water fluoridation represents an important public health prevention target.
Conclusions
Clear gradients of social inequalities for child dental caries exist across four high-income countries in this study. Variation in the prevalence of child dental caries and the extent of social inequalities across jurisdictions suggest that each may be responsive to oral health policy. The achievable combination of universal dental insurance and care (which includes adults/parents and children) and water fluoridation may be the necessary policy levers to achieve lower and more equitable rates of dental caries. To differentially benefit socio-economically disadvantaged groups of children, and sustain subsequent longer-term adult health benefits, it is timely to consider these universal and powerful public health measures in order to deliver on the aspirations of the WHO global oral health strategy.
*Original full-text article online at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0268899
