Full-text study online here
PDF of study online here
Published: September 30, 2021
Abstract
Introduction
Dental caries is a global health issue. It is a largely preventable, multifactorial non-communicable disease. Given the gravity of the situation, in 2014 United States Preventive Services Task Force recommended that the primary care physician apply fluoride varnish from the eruption of the first tooth till the child attains five years of age. Using 2016-2019 National Survey of Children’s Health (NSCH) cross-sectional representative data, the aim of this study was to determine if the child’s age, gender, and race are predictors of the child having decayed teeth or cavities in the past 12 months and if they had availed preventative dental services from the dentist in the past 12 months in the US and if so, did they receive fluoride treatment.
Methods
The prevalence of dental caries and dental treatment among children under each category of sociodemographic risk factors were estimated using 2016-2019 NSCH’s cross-sectional representative data on two survey questions. Then, the statistical significance of the association of the categorical risk factors with the prevalence of dental caries and the association of the categorical risk factors with the prevalence of fluoride dental treatment were tested using two-sample proportion tests and chi-square tests. Further, chi-square residual analysis was employed to better understand the nature of the association and to reveal the degree of contribution to the test statistic from each categorical combination of risk factors.
Results
Prevalence and associative risk of tooth decay in children was the highest in the 6-11 years age group across all three years under study. The 6-11 years age group had the highest prevalence and association of receiving fluoride treatment across all three years. In our study, the prevalence of dental caries in children by race varied according to the year. In 2016-2017 and 2018-2019, it was the Hispanic population with the highest prevalence of tooth decay. In 2017-2018 the highest prevalence was seen in the Non-Hispanic Black (NHB) population. Across all three years, the Hispanic population had the highest associative risk of tooth decay. The Non-Hispanic White (NHW) population had the highest prevalence and association with receiving fluoride treatment across all three years. Male children were found to have the higher prevalence and associative risk of decayed teeth across all three survey years.
Conclusion
Dental caries is a worldwide health burden. However, it can be prevented by different precautionary measures. The results of our study revealed that certain sociodemographic factors such as age, gender, and race of the child make certain groups of the child population more at risk for the development of dental caries; most notable findings were that the male children were significantly associated to have decayed teeth and not availing dental fluoride treatment for which limited information is available in the literature. Additionally, the age groups 1-5 and 6-11 were significantly associated with the prevalence of not receiving dental treatment and the prevalence of dental caries, respectively. More active participation of pediatricians in getting trained for the application of fluoride varnish and helping getting their patients established with dental services per recommendations will help streamline preventative dental care.
Introduction
Dental caries is a global health issue. It is a largely preventable, multifactorial non-communicable disease. Several pathological factors responsible for dental caries are cariogenic pathogens, fermentable carbohydrates, and a longer time of exposure among others. Saliva, fluoride, plaque control, and carbohydrate intake control serve as protective factors. Oral microbiota form a dental biofilm on the tooth surface that serves as the habitat for cariogenic bacteria [1]. Through pH-driven changes in the oral fluid, fluoride through topical effect helps in remineralization of the tooth enamel and prevents demineralization of it as it stays in the saliva for a certain period of time [2,3]. This helps prevent tooth decay which occurs due to pH changes caused by cariogenic bacteria fermenting carbohydrates. The recommended daily adequate intake of fluoride is the same for males and females from ages birth to 18 years of age and the intake varies per age group. For 0-6 months, 7-12 months, 1-3 years, 4-8 years, 9-13 years, and 13-18 years age groups the daily adequate intake in milligrams (mg) is 0.01, 0.50, 0.70, 1.00, 2.00, and 3.00, respectively [4].
Water fluoridation has been a successful intervention over the years in the prevention of dental caries. Fluoride-containing toothpastes have been another efficient vehicle of delivery of fluoride worldwide [5]. According to a study by Walsh et al. different parts per million fluoride concentration toothpastes had different caries preventive effects [6]. The United States Public Health Service had provided recommendations with updates since 1962 on optimal fluoride concentrations through community water systems to prevent dental caries. The current recommendation being 0.7 milligrams/liter of fluoride [7]. The percentage of the population that receives fluoridated water through community water systems has steadily increased from 37.3% in 1964 to 73% by 2018 [8]. In a study by Dye et al. dental caries was found to be the most chronic and preventable disease in children of age group 6-11 years and in adolescents between 12-19 years [9].
Given the gravity of the situation, in 2014 United States Preventive Services Task Force (USPSTF) recommended that the primary care physician apply fluoride varnish from the eruption of the first tooth till the child attains five years of age. It is to be applied two to four times per year [10,11]. It is a B-level recommendation where there is fair level evidence it improves important health outcomes and benefit outweighs harm [12]. Our objective for this study was to determine using 2016-2019 National Survey of Children’s Health’s (NSCH) cross-sectional representative data, if the child’s age, gender, and race are predictors of the child having decayed teeth or cavities in the past 12 months and if they had availed preventative dental services from the dentist in the past 12 months in the US and if so, did they receive fluoride treatment.
Materials & Methods
Data sources
The NSCH is a nationwide survey designed to acquire national and state-level prevalence estimates of the physical and emotional health of children aged 0-17 years. The NSCH is sponsored by the Health Resources and Services Administration and Maternal and Child Health Bureau [13]. The survey is executed as part of the State and Local Area Integrated Telephone Survey by the Centers for Disease Control and Prevention, National Center for Health Statistics. The selection process includes a random data collection of one child under age eighteen from each household where the respondent is an adult in the household who is knowledgeable about the child’s health.
The data were collected nationally by sending mail invites to fill online or paper surveys by parents/guardians of children aged 1-17 years by NSCH. A total of 131,774 subjects’ level topical questionnaires data were collected and pre-processed (Table 1).
| Year of survey |
2019 |
2018 |
2017 |
2016 |
| Number of children completing the questionnaires |
29,433 |
30,530 |
21,599 |
50,212 |
The analysis was conducted on this cross-sectional representative data collected from 2016-2019.
Study measures
The association of the categorical risk factors such as age, gender, and race with the prevalence of dental caries and the prevalence of fluoride dental treatment among children aged 1-17 years were investigated based on the responses given for the following survey questions provided in NSCH data (2016-2017, 2017-2018, 2018-2019).
1. “During the past 12 months, has this child had decayed teeth or cavities, age 1-17 years?”
2. “During the past 12 months, what preventive dental services did this child receive: fluoride treatment, age 1-17 years?”
Statistical analysis
Inter-group differences in abundance were evaluated using Z-proportion tests for dichotomous categorical variables and two-way chi-square (?2) tests for non-dichotomous categorical variables. The chi-square test, which evaluates the significant association between the mutually exclusive categories of the multiple variables, was employed [14,15]. For the first survey question, the contingency table is constructed with rows having categories of sociodemographic factors as provided in Table 2 and the columns having the categories namely children having decayed teeth (TD) and not having decayed teeth (NTD).
| Study variable |
Study categories used |
| Gender |
1. Male 2. Female |
| Age (yrs) |
1. 1-5 2. 6-11 3. 12-17 |
| Race/ethnicity |
1. Hispanic 2. NHW 3. NHB 4. NHA 5. NHO |
For the second survey question, the rows of the contingency table were categories of each sociodemographic factor and the columns were three categories of dental treatment namely received fluoride treatment (RF), received treatment without fluoride (RNF), and not received treatment (NR), respectively. The null hypothesis (H0) of the chi-square test is that no association exists on the categorical variables in the population and they are independent. Larger values of ?2 test statistics are more contradictory to H0. In a similar way, smaller p-value (< 0.05) is contradictory to H0 where p-value is the null probability that ?2 is at least as large as the observed value.
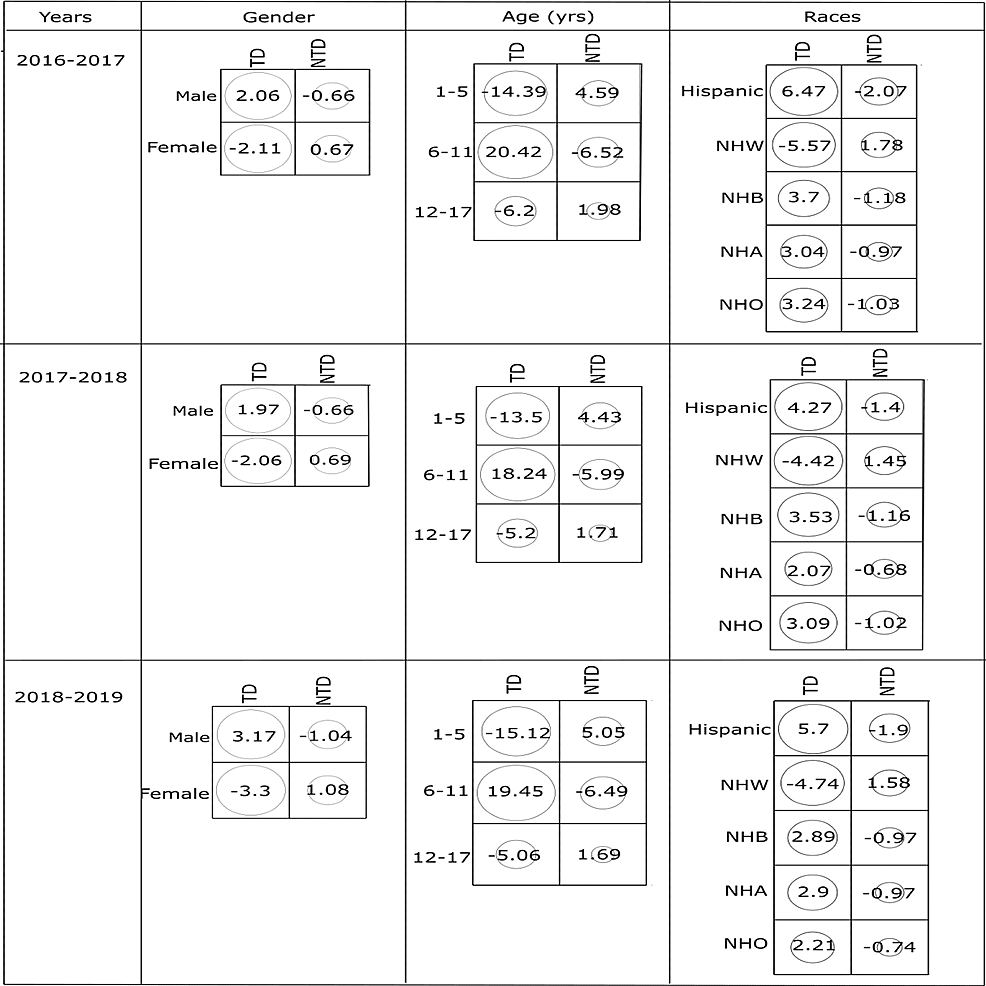
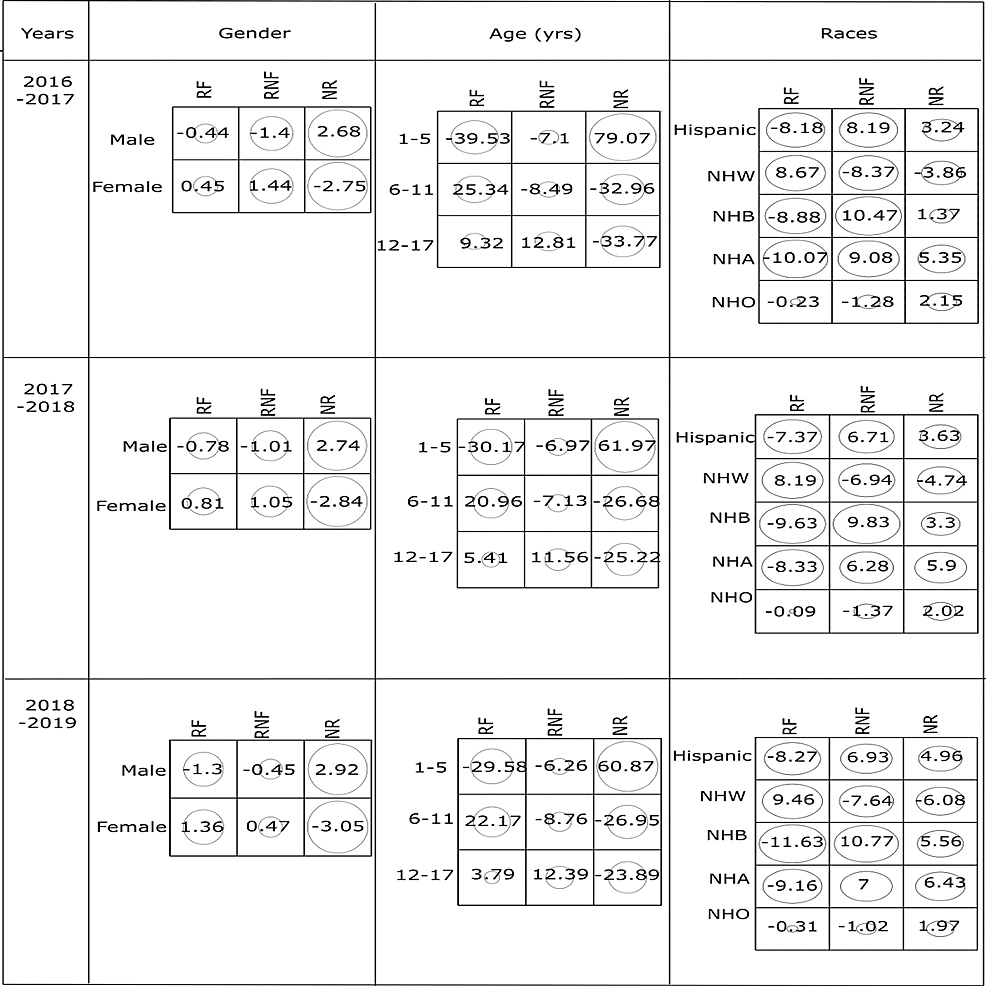
Further, once an association between categorical variables through the chi-square test is established, residual analysis was utilized to identify the degree of contribution to the test statistic from each categorical combination [16,17]. The standardized residuals which are measures of how significant the cells in the contingency table are to the chi-square value, are calculated. A cell-by-cell comparison of observed frequency (count) and the expected frequency which is based on H0 can help to better understand the nature of the association. The larger the positive residuals of the cell, the higher the count and larger the negative residuals, the fewer the count of the categorical combination relevant to the particular cell than what the hypothesis of independence predicts [18]. Therefore, the larger positive residuals and negative residuals indicate a stronger positive and stronger negative association between the categories of each cell respectively. Statistical analyses and information visualizations were performed using R software (version 4.0.0) [19]. All plots were produced using the packages ‘stats’ and ‘corrplot’.
Results
Table 3 shows a basic comparison of the children having dental caries and not having dental caries with the sociodemographic risk factors based on the first survey question.
| Variables |
Categories |
Possess dental caries, Total number-n, Prevalence (%) |
?2 value |
p-value |
| Having teeth-decay n (%) |
Not having teeth-decay n (%) |
| 2016-2017 |
| Gender |
Male |
3353 (9.59) |
31,612 (90.41) |
9.49(a) |
0.001 |
|
Female |
2962 (8.90) |
30,308 (91.10) |
|
|
| Age (yrs) |
1-5 |
1062 (5.97) |
16,719 (94.03) |
176.80(b) |
<0.001 |
|
6-11 |
2874 (13.51) |
18,392 (86.49) |
|
|
|
12-17 |
2379 (8.15) |
26,809 (91.85) |
|
|
| Race |
Hispanic |
874 (11.51) |
6717 (88.49) |
729.92(b) |
<0.001 |
|
NHW |
4045 (8.48) |
43,661 (91.52) |
|
|
|
NHB |
447 (11.02) |
3609 (88.98) |
|
|
|
NHA |
391 (10.79) |
3233 (89.21) |
|
|
|
NHO |
558 (10.61) |
61,920 (89.39) |
|
|
| 2017-2018 |
|
|
|
|
|
| Gender |
Male |
2686 (10.36) |
23,252 (89.64) |
23.06(a) |
<0.001 |
|
Female |
2181 (9.08) |
21,848 (90.92) |
|
|
| Age (yrs) |
1-5 |
776 (6.03) |
12,099 (93.97) |
600.33(b) |
<0.001 |
|
6-11 |
2252 (14.27) |
13,528 (85.73) |
|
|
|
12-17 |
1839 (8.63) |
19,473 (91.37) |
|
|
| Race |
Hispanic |
669 (11.49) |
5155 (88.51) |
70.98(b) |
<0.001 |
|
NHW |
3108 (9.00) |
31,434 (91.00) |
|
|
|
NHB |
373 (11.69) |
2818 (88.31) |
|
|
|
NHA |
271 (11.04) |
2183 (88.96) |
|
|
|
NHO |
446 (11.27) |
3510 (88.73) |
|
|
| 2018-2019 |
| Gender |
Male |
3132 (10.39) |
27,020 (89.61) |
8.95(a) |
0.001 |
|
Female |
2661 (9.64) |
24,956 (90.36) |
|
|
| Age (yrs) |
1-5 |
899 (6.09) |
13,870 (93.91) |
703.12(b) |
<0.001 |
|
6-11 |
2671 (14.58) |
15,651 (85.42) |
|
|
|
12-17 |
2223 (9.01) |
22,455 (90.99) |
|
|
| Race |
Hispanic |
837 (12.21) |
6020 (87.79) |
85.10(b) |
<0.001 |
|
NHW |
3714 (9.28) |
36,315 (90.72) |
|
|
|
NHB |
427 (11.53) |
3275 (88.47) |
|
|
|
NHA |
328 (11.77) |
2459 (88.23) |
|
|
|
NHO |
487 (11.08) |
3907 (88.92) |
|
|
The following are the notable observations about the prevalence estimation of dental caries among children under categories of each risk factor. The prevalence of dental caries among male children was 9.59%, 10.36%, 10.39% in 2016-2017, 2017-2018, 2018-2019 respectively which is higher compared to the prevalence of dental caries among female children. Among children aged 1-17 years, the prevalence of dental caries was highest for the 6-11 age category in all three years. When considering the race risk factor, the higher prevalence of dental caries varied as Hispanic (11.51%), Non-Hispanic Black (NHB) (11.69%), Hispanic (12.21%) in the respective years 2016-2017, 2017-2018, and 2018-2019. Based on these preliminary results of prevalence estimation, the statistical significance of the differences in the prevalence of dental caries under each category of risk factors was tested.
The risk factor gender was categorized as a dichotomous variable with male and female as two categories. Therefore, the two-sample proportion test was used and the results show significant association (p < 0.001) between the prevalence of dental caries among males and females. For the non-dichotomous variables age and race, the chi-square test was used. The results indicated both age and race contradict (p < 0.001) with H0 and implying significant association with the prevalence of dental caries. Overall, Table 3 results depict that significant statistical associations exist between sociodemographic risk factors and prevalence of dental caries for all three years (2016-2017, 2017-2018, 2018-2019).
Since the two-sample proportion test and chi-square results show the statistically significant association, the strength of association between the risk factors and prevalence of dental caries was further explored using the standard residuals as shown in Figure 1.
The highest positive value of residuals (?