This guidance is issued jointly by the Department of Health and Social Care, the Welsh Government, the Department of Health Northern Ireland, Public Health England, NHS England and NHS Improvement and with the support of the British Association for the Study of Community Dentistry.
Delivering Better Oral Health has been developed with the support of the 4 UK Chief Dental Officers.
Whilst this guidance seeks to ensure a consistent UK wide approach to prevention of oral diseases, some differences in operational delivery and organisational responsibilities may apply in Wales, Northern Ireland and England. In Scotland the guidance will be used to inform oral health improvement policy.
Fluoride and dental caries prevention
Fluorides are widely found in nature and in products such as tea, fish, beer and in some natural water supplies. The link between fluoride in public water supplies and reduced levels of dental caries was first documented early in the last century. Since then fluoride has become more widely available, most notably in toothpaste, and recognised as having improved oral health in the UK. The decline of dental caries worldwide over recent decades is largely attributed to the daily use of fluoride toothpaste (1).
There is abundant evidence that increasing fluoride availability to individuals and communities is effective at reducing dental caries levels (Chapter 2: Table 1; Chapter 4). For example, moving from brushing once a day to twice a day lowers an individual’s risk of developing dental caries by 14% (2).
Regular exposure to fluoride maintains a concentration in the plaque biofilm that encourages remineralisation of the tooth surface. This can be achieved by a range of methods, but similar principles apply to all. Fluoride delivery using vehicles that can be incorporated into aspects of everyday living are more likely to be effective and they avoid increasing inequalities.
The risk of ingesting too much fluoride leading to fluorosis should be considered for young children during tooth formation (3). A balance has to be achieved, whereby, most benefit can be gained from this naturally occurring substance, whilst at the same time minimising the risk of fluorosis.
Water fluoridation
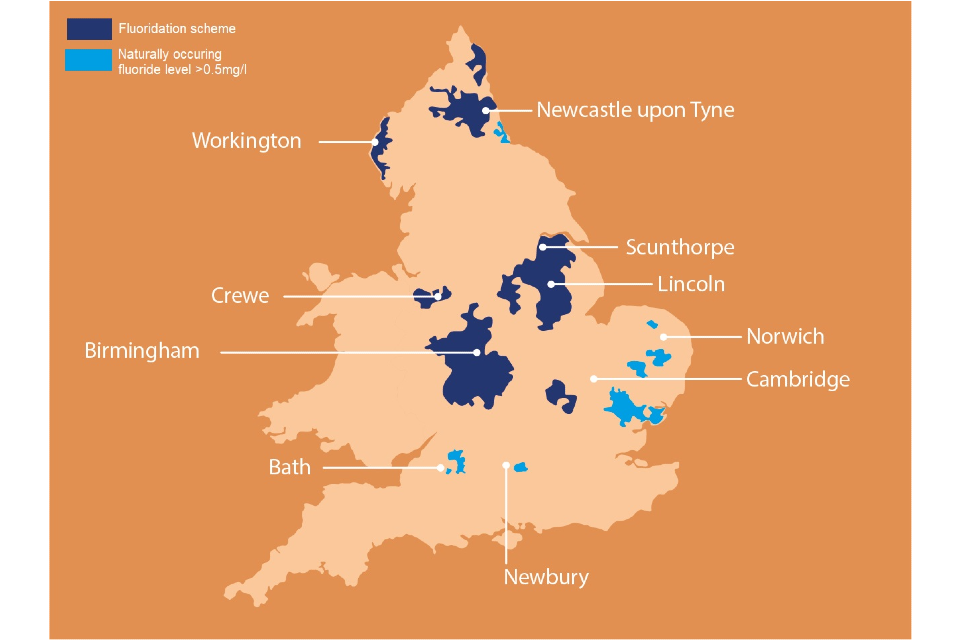
Currently, approximately 10% of England’s population, or about 6 million people, have a fluoridatated water supply. In terms of population coverage, the West Midlands is the most extensively fluoridated area, followed by parts of the North East of England (Figure 9.1).
There are no fluoridation schemes in Scotland, Wales and Northern Ireland, however, there are some localised areas of naturally occurring fluoride in the water. To check if the water supply in a given area is fluoridated, information can be obtained from the local water supplier by quoting the residential postcode. Many water companies have an online function to allow consumers to check the level of fluoride.
Milk fluoridation
There are a few community schemes in England which supply children with fluoridated milk at early years and school settings. They are provided in areas that are not fluoridated and where levels of dental caries are high. In 2016 an evidence review and guide for local authorities commissioning programmes such as fluoridated milk classified these as of limited value for oral health (4).
Increasing fluoride availability
Information on how fluoride availability can be increased on an individual basis to improve oral health follows below. This can involve a range of behaviours and modes of delivery, linking closely, but not exclusively, to oral hygiene practices. Concentration, frequency and mode of delivery of fluoride are important, together with practical action to ensure that fluoride stays in the oral cavity and is not rinsed away.
Fluoride toothpaste
Toothpaste is the most common delivery system for fluoride and comes in a range of strengths, flavours and formulations. For further details on toothbrushing please see Chapter 8 on oral hygiene . There is moderate to high-certainty evidence that fluoride toothpaste of 1,000 ppm fluoride or above prevents dental caries in both the permanent and primary dentition (5). For children at higher risk, 1,350 to 1,500 ppm is advocated and also for children from 7 years upwards (5).
The formulation of fluoride in toothpaste varies and can take various forms, for example, sodium fluoride, sodium monofluorophosphate, stannous fluoride, or a combination of these. However, currently, there is insufficient evidence to confidently recommend one over another. It is the strength in parts per million fluoride (which can be found on the packaging) that is important (5), along with consideration of wider dental caries risk factors, particularly sugar in the diet.
It is important to brush at least twice a day with fluoride toothpaste, last thing at night or before bedtime and one other time (5, 6). It is also helpful to recognise that a combination of health behaviours such as using higher fluoride paste, brushing twice a day and avoiding rinsing after brushing appears to be associated with reducing the dental caries increment in adolescents (2).
Types of over-the-counter toothpastes by fluoride concentration level
A table of currently available toothpastes and their fluoride content is provided for information. The list is not an endorsement of any particular brand. Whilst every effort has been made to ensure the list is comprehensive, and correct at the time (January 2020), it may not represent all brands of toothpaste available in the UK. Analysis of toothpastes suggested that almost one-third (31%) of available toothpastes contained no fluoride and 4% had an unrecorded concentration (7). Information is not available about levels of fluoride in brands bought from places such as single price stores, markets, websites and car boot sales, which may be special imports or, on occasion counterfeit, and not contain any fluoride. Such toothpaste may not offer protection against dental caries. There is increasing diversity in the toothpaste market with greater emphasis on whitening, natural, and holistic health products. This trend highlights the importance of dental professionals taking time to recognise the changing market, explore with patients what toothpastes they are using, and why, in order to assist them in selection of an appropriate product.
Higher dose fluoride toothpaste
The maximum concentration of fluoride-containing toothpaste that can be purchased over the counter in the UK is 1,500 ppm fluoride. Higher dose toothpastes are available on prescription from a dentist. Evidence on the efficacy of higher dose fluoride toothpastes is limited (5) and available studies focus on root caries (8). Dentists may wish to consider higher concentration fluoride toothpastes for vulnerable young people and adults susceptible to dental caries (9). Dental caries risk should be reviewed at routine oral health assessments and high fluoride toothpaste only continued for those who are unable to reduce their susceptibility to dental caries.
Prescribing higher dose fluoride toothpaste
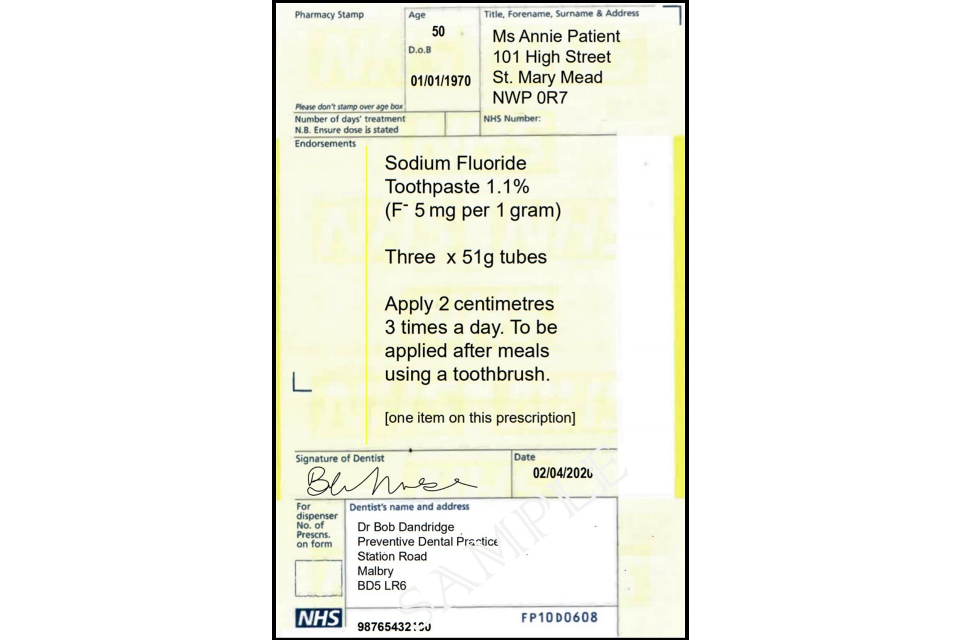
The following sections provide information and advice on fluoride prescription including examples of prescription scripts. It is important to avoid chronic and/or acute ingestion of fluoride; however, occurrences of excessive fluoride ingestion in adults from high fluoride toothpastes are very rare (10). Adults should be advised to follow the instructions under which these medications are licensed which recommends a 2cm ribbon on toothbrush head 3 times daily. As with children, adults should be encouraged to spit out excess toothpaste and avoid rinsing. Adults with limited capacity should be supported in toothbrushing to ensure that they use the recommended amount only.
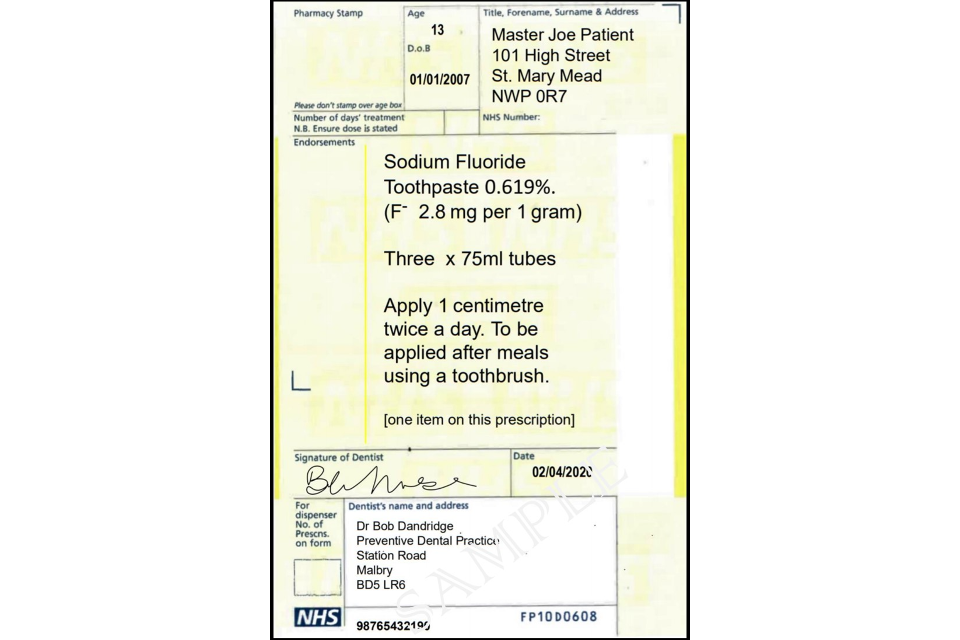
Sodium fluoride 2,800 ppm fluoride toothpaste
Indications for use include high dental caries risk patients aged 10 years and over. This includes those with dental caries present, a high cariogenic diet or cariogenic medication. Whilst this approach may be helpful as dental caries risk is tackled, most patients will benefit from reducing their sugar intake in the longer term. However, it may be necessary to continue with high fluoride toothpaste where patients are unable to reduce their susceptibility to dental caries. For example of a prescription, please see Figure 9.2 below.
Sodium fluoride 5,000 ppm toothpaste
Indications for use include high dental caries risk patients aged 16 years and over. This includes those with root or coronal caries present or risk factors such as dry mouth, overdentures, those with a highly cariogenic diet or cariogenic medication and those who have received head and neck radiotherapy and chemotherapy (5, 11). Again, this should be used in conjunction with reducing sugar intake, subject to review and not normally for the long term, except in specific circumstances. For example of a prescription please see Figure 9.3 below.
Toothpaste taste, texture and foaming
The taste of toothpaste varies between brands and countries and is influenced by the target market. While fruit flavoured toothpastes aimed at children are available, as the majority of family toothpastes are mint flavoured, it is recommended to start young children on a mild mint family toothpaste. If fruit flavoured toothpastes are chosen, extra care must be taken to ensure that children do not eat or swallow the toothpaste because they like the taste. Transition to mint flavoured paste should therefore be encouraged as soon as the child will tolerate this taste.
Toothpaste taste can be a barrier to regular use, particularly in children with sensory sensitivities, including autism and learning disabilities who may benefit from a paste that is less flavoured or foaming.
People who have a vulnerable airway, for example if they have experienced a stroke or are on a ventilator, or some adults and children with special needs (such as sensory sensitivities, dysphagia, dry mouth, cognitive decline, having nil by mouth) will benefit from a toothpaste that produces less foam (12, 13). Thus they would benefit from toothpaste that is free from sodium lauryl sulphate. Examples of such products can be found in the Mouthcare Matters product list.
Fluoride varnish
Fluoride varnish is one of the best options for increasing the availability of topical fluoride regardless of the levels of fluoride in any water supply (14). This should happen when a child visits a dental surgery and is strongly recommended (14). The dental caries-preventive effectiveness of fluoride varnish in both permanent and primary dentitions is clear (14, 15). Several systematic reviews conclude that applications twice a year produce an average reduction in dental caries increment of 37% in the primary and 43% in the permanent dentition (14). Much of the evidence of effectiveness is derived from studies which have used sodium fluoride 22,600 ppm (2.26% NaF) varnish for application.
Fluoride varnish for use as a topical treatment has several practical advantages. It is well accepted and safe for most patients (see exceptions below). Furthermore, the application of fluoride varnish is simple and can be applied by trained and competent members of the oral healthcare team including dental nurses. While a thorough prophylaxis is not essential prior to application, removal of gross plaque is advised. Dental nurses can be trained to apply fluoride varnish to the prescription of a dentist and this use of team skill mix can assist a practice to become more preventively orientated (16). A detailed protocol for the application of fluoride varnish is currently available from the Scottish Childsmile Manual (17, 18).
The use of fluoride varnish is contraindicated in patients with ulcerative gingivitis and stomatitis (19). There is a very small risk of allergy to one component (colophony) of the most commonly used fluoride varnish. Check any medical history with the parent, specifically check for allergy to sticking plaster or severe allergy or asthma that has required hospitalisation (17), the use of colophony containing varnish application is contraindicated for these cases. Other brands of varnish may have different constituents.
Some fluoride varnishes contain alcohol. Because they are being used as a medicament and are not an intoxicant, it has been agreed (on the authority of the West Midlands Shari’ah Council) that they are suitable for use by Muslims, provided that they are used in small amounts, well below that which would intoxicate, and they are not being used for reasons of vanity.
Clinicians should be aware that many fluoride varnishes on the market are not licensed for dental caries control, although they may have similar formulations, and take this into consideration with respect to their prescribing responsibilities. Practitioners need to be aware of their responsibilities when prescribing off-licence, and should ensure that they are in the best interests of the patient and taking account of product availability (20).
Whilst most of the focus on fluoride varnish use has been on dental caries prevention in children, it is increasingly important to consider its use with adults at higher risk, particularly frail older people, who have maintained their natural teeth. Fluoride varnish has the advantage of being professionally applied and does not have aesthetic challenges.
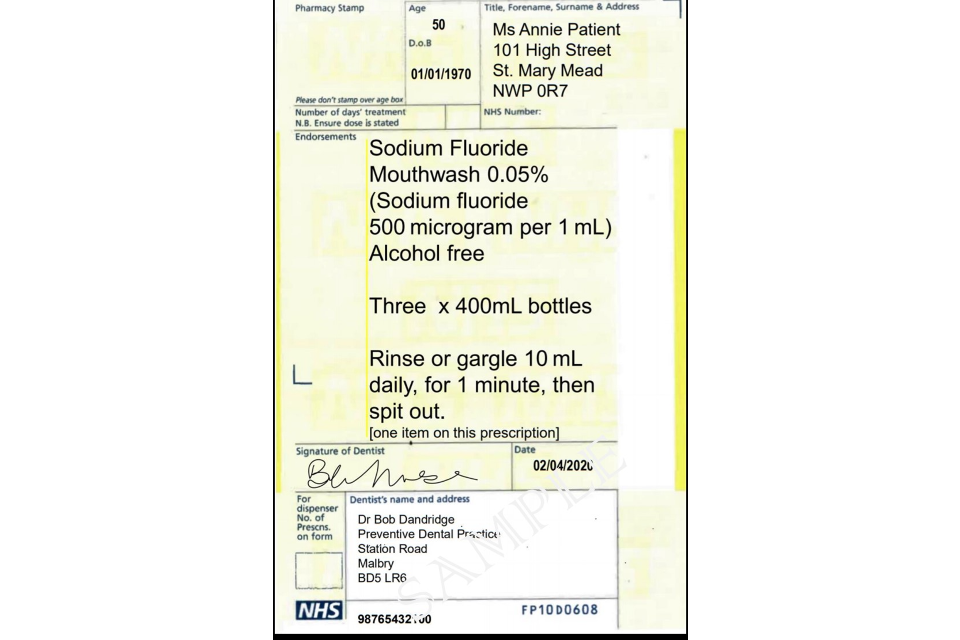
Fluoride mouthwashes
Fluoride mouthwashes or mouthrinses (0.05% w/v; 230 ppm) can be considered for patients aged 8 years and above, for daily use, in addition to twice daily brushing with toothpaste containing at least 1,350 ppm fluoride (21). Rinses require patient compliance and should be used at a different time to toothbrushing to maximise the topical effect which enhances the bioavailability of fluoride in the plaque biofilm (22). They are likely to be most useful in higher dental caries risk patients.
There is moderate-certainty evidence that fluoride mouthrinses prevent dental caries in the permanent dentition, although the evidence is derived from supervised use at school (21). There are no trials of the effect of mouthrinses on the primary dentition.
Overall, there is insufficient evidence to support daily (230ppm) versus weekly (circa 900ppm) mouthwash use as superior, in terms of dental caries prevention (21). The available evidence coming from school-based programmes where children are supervised suggests that regular use of fluoride mouthrinse results in a large reduction in tooth decay in the permanent teeth of children and adolescents. The benefit of fluoride mouthrinse is likely to be present even if children use fluoride toothpaste or live in water?fluoridated areas (21). For an example of a prescription, please see Figure 9.4 below.
Fluorides and the risk of dental fluorosis
A potential side effect of using fluoride as a dental caries-preventive measure is the occurrence of dental fluorosis, which can occur if a child is exposed to excess ingested fluoride during the period of tooth formation (23).
The risks of fluorosis damaging the appearance of permanent incisors are relevant only to ingestion of fluoride by those under 3 years old (17, 24), as calcification of the crowns of permanent incisor teeth is complete by 30 months.
Risks of aesthetically challenging fluorosis to premolars are only relevant to those aged under 6 years as calcification of the crowns of these teeth is complete by this age. To minimise risk of fluorosis, while still using the optimum concentration of fluoride in toothpaste (5), the best approach is to use very small quantities for children aged 6 years and below, whilst teeth are still calcifying.
Children aged under 3 years
Parents of children aged under 3 years are advised to have only a smear of fluoride toothpaste (3), when toothbrushing (Chapter 8) while their incisors are forming, as shown in Figure 9.5a below.
If a smear of 1,000 ppm toothpaste is used, this amounts to 0.1ml of paste by volume which contains 0.1mg of fluoride.
When 1,500 ppm paste is used the ‘smear’ (0.1ml) of paste contains 0.15mg of fluoride.
Overall, this results in an absorbable fluoride dose of only 0.007 to 0.01mg per kg body weight if swallowed, for a child weighing 15kg (17).

Children aged 3 to 6 years
Children aged 3 to 6 years should use only a pea-sized blob of toothpaste (3) when teeth are being brushed (Chapter 8) as shown in Figure 9.5b below.
If a pea-sized blob of 1,000 ppm toothpaste is used, this amounts to 0.25ml of toothpaste containing 0.25mg of fluoride.
When 1,500 ppm paste is used the ‘pea’ (0.25ml) of toothpaste contains 0.375mg of fluoride.
Overall this results in an absorbable fluoride dose of only 0.02 to 0.025mg per kg body weight if swallowed, for a child weighing 15kg (17).

Deciding on fluoride delivery options
Fluoride should form part of the standard tools to tackle dental caries and reduce risk. Standard, age-appropriate advice should be given to everyone, that is, toothbrushing with fluoride toothpaste (1,350 to 1,500 ppm) (5). Additional action for patients who are at higher risk of dental caries should involve careful consideration based on their history, area of residence, clinical examination and special investigations such as diet diary. Higher fluoride paste (over 1,500 ppm toothpaste) should ideally be a short-term risk reduction measure whilst the level of sugar in the diet is reduced. Exceptions will include patients who are at higher long-term risk of dental caries. This may be because of reduced salivary flow, physical or learning disability or medical conditions.
Other dental caries-preventive agents
Novel and emerging products
New toothpastes and equivalent products are emerging on the market. They include toothpaste tablets (7), albeit supported by limited or no evidence regarding their effectiveness. Some of these products do not contain fluoride and are driven by a desire for natural products and also environmental sustainability (7). It is likely that more products will emerge, and oral healthcare professionals are encouraged to check them on a regular basis, particularly to check if they contain fluoride. Where patients have elected to use a non-fluoride toothpaste, it is important to highlight the loss of dental caries preventive effect and the increased need to manage their sugar intake to prevent dental caries.
Fluoride in combination with other preventive agents
One systematic review focused on preventive dental regimes and/or one or more chemical agents applied by a dental professional to reduce the initiation of root caries lesions or render them inactivate (11). It highlighted that dentifrice containing 5,000 ppm fluoride, and professionally applied chlorhexidine or silver diamine fluoride varnish, may inactivate existing decay and/or reduce the initiation of root caries lesions (low-certainty evidence). However, the results should be interpreted with caution, due to the low numbers of clinical trials for each agent, the high risk of bias within studies, and the limiting grade of evidence.
Recent reviews have highlighted the benefits of Silver diamine fluoride (SDF) in dental caries management (25, 26), albeit the quality of evidence is low. Silver diamine fluoride, however, is licensed in the UK for management of dentine hypersensitivity, not the prevention or arrest of dental caries. An emerging body of evidence suggests that it is a useful vehicle for fluoride delivery with the evidence consistently supporting SDF’s effectiveness for arresting coronal caries in the primary dentition and root caries in older adults for all comparators (26). SDF can arrest established carious lesions, especially in primary teeth (25, 26); however, it blackens teeth and so has challenging aesthetic properties. There is also emerging evidence that it may be beneficial in preventing further root caries in older people (25, 26).
Further high quality research is therefore required to determine its potential beyond its current product licence, including investigating its primary preventive properties and the most beneficial time intervals for its use. Thus, whilst there is some suggestion that SDF is effective in dental caries prevention as an agent in young children (25), and possibly for root caries in older adults, current evidence essentially focuses on caries arrest.
Resources
Simple communication tool to support fluoride varnish application (In the Dentist’s Room).
References
1. Pitts NB, Zero DT, Marsh PD, Ekstrand K, Weintraub JA, Ramos-Gomez F and others. Dental caries. Nature Reviews Disease Primers. 2017;3:17030.
2. Chesters RK, Huntington E, Burchell CK, Stephen KW. Effect of oral care habits on caries in adolescents. Caries Research. 1992;26(4):299-304.
3. Wong MCM, Glenny AM, Tsang BWK, Lo ECM, Worthington HV, Marinho VCC. Topical fluoride as a cause of dental fluorosis in children. Cochrane Database of Systematic Reviews. 2010(1).
4. Public Health England. Local authorities improving oral health: commissioning better oral health for children and young people: An evidence-informed toolkit for local authorities. London: Public Health England; 2014.
5. Walsh T, Worthington HV, Glenny AM, Marinho VCC, Jeroncic A. Fluoride toothpastes of different concentrations for preventing dental caries. Cochrane Database of Systematic Reviews. 2019(3).
6. SIGN. Sign 138. Dental interventions to prevent caries in children. Health Improvement Scotland; 2014.
7. Gupta A, Godson J, Chestnutt IG, Gallagher J. Formulation and fluoride content of dentifrices: A review of current patterns. British Dental Journal. in press.
8. Wierichs RJ, Meyer-Lueckel H. Systematic Review on Noninvasive Treatment of Root Caries Lesions. Journal of Dental Research. 2014;94(2):261-71.
9. Public Health England. Commissioning better oral health for children and young people: An evidence-informed toolkit for local authorities. London: Public Health England; 2018.
10. Randall C. Fluoride toothpaste – what are the dangers of chronic ingestion in adults? In: Service SP, editor. Dentistry 2019.
11. Wierichs RJ, Meyer-Lueckel H. Systematic review on noninvasive treatment of root caries lesions. Journal of Dental Research. 2015;94(2):261-71.
12. Smith CJ, Horne M, McCracken G, Young D, Clements I, Hulme S and others. Development and feasibility testing of an oral hygiene intervention for stroke unit care. Gerodontology. 2017;34(1):110-20.
13. Prendergast V, Kleiman C, King M. The Bedside Oral Exam and the Barrow Oral Care Protocol: translating evidence-based oral care into practice. Intensive and Critical Care Nursing. 2013;29(5):282-90.
14. Marinho VCC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews. 2013(7).
15. Mishra P, Fareed N, Battur H, Khanagar S, Bhat MA, Palaniswamy J. Role of fluoride varnish in preventing early childhood caries: A systematic review. Dental Research Journal (Isfahan). 2017;14(3):169-76.
16. Chief Dental Officer England. Avoidance of Doubt-Application of Fluoride Varnish by Dental Nurses. In: Officer OotCD, editor. London: NHS England; 2016.
17. NHS Scotland, Healthier Scotland. Programme Manual for Childsmile Staff. Glasgow: University of Glasgow; 2016. Contract No.: 4531.
19. Colgate. Colgate Duraphat Varnish: product leaflet 2020
20. MHRA. Off-label or unlicensed use of medicines: prescribers’ responsibilities: UK Govenment; 2014 [updated 11 December 2014].
21. Marinho VCC, Chong LY, Worthington HV, Walsh T. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews. 2016(7).
22. Weyant RJ, Tracy SL, Anselmo TT, Beltrán-Aguilar ED, Donly KJ, Frese WA and others. Topical fluoride for caries prevention: executive summary of the updated clinical recommendations and supporting systematic review. Journal of the American Dental Association. 2013;144(11):1279-91.
23. Buzalaf M, Levy S. Fluoride Intake of Children: Considerations for Dental Caries and Dental Fluorosis. Monographs in oral science. 2011;22:1-19.
24. Wright JT, Hanson N, Ristic H, Whall CW, Estrich CG, Zentz RR. Fluoride toothpaste efficacy and safety in children younger than 6 years: a systematic review. Journal of the American Dental Association. 2014;145(2):182-9.
25. Oliveira BH, Rajendra A, Veitz-Keenan A, Niederman R. The Effect of Silver Diamine Fluoride in Preventing Caries in the Primary Dentition: A Systematic Review and Meta-Analysis. Caries research. 2019;53(1):24-32.
26. Seifo N, Cassie H, Radford JR, Innes NPT. Silver diamine fluoride for managing carious lesions: an umbrella review. BMC Oral Health. 2019;19(1):145.
*Original online at https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention/chapter-9-fluoride
