Abstract
- Supplementary File 1: ZIP-Document (ZIP, 7609 KiB)
References
- Cheng, L.; Zhang, K.; Zhang, Z. Effectiveness of thiazides on serum and urinary calcium levels and bone mineral density in patients with osteoporosis: A systematic review and meta-analysis. Drug Des. Dev. Ther. 2018, 12, 3929–3935. [Google Scholar] [CrossRef]
- Cummings, S.R.; Melton, L.J. Epidemiology and outcomes of osteoporotic fractures. Lancet 2002, 359, 1761–1767. [Google Scholar] [CrossRef]
- Vidal, M.; Thibodaux, R.J.; Neira, L.F.V.; Messina, O.D. Osteoporosis: A clinical and pharmacological update. Clin. Rheumatol. 2019, 38, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Sattui, S.E.; Saag, K.G. Fracture mortality: Associations with epidemiology and osteoporosis treatment. Nat. Rev. Endocrinol. 2014, 10, 592–602. [Google Scholar] [CrossRef] [PubMed]
- Daruwalla, Z.J.; Huq, S.S.; Wong, K.L.; Nee, P.Y.; Leong, K.M.; Pillay, K.R.; Murphy, D.P. Hip fractures, preceding distal radius fractures and screening for osteoporosis: Should we be screening earlier? A minimum 10-year retrospective cohort study at a single centre. Osteoporos. Int. 2016, 27, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Willson, T.; Nelson, S.D.; Newbold, J.; Nelson, R.E.; LaFleur, J. The clinical epidemiology of male osteoporosis: A review of the recent literature. Clin. Epidemiol. 2015, 7, 65–76. [Google Scholar]
- Silverman, S.L.; Kupperman, E.S.; Bukata, S.V. Fracture healing: A consensus report from the International Osteoporosis Foundation Fracture Working Group. Osteoporos. Int. 2016, 27, 2197–2206. [Google Scholar] [CrossRef]
- Unni, S.; Yao, Y.; Milne, N.; Gunning, K.; Curtis, J.R.; LaFleur, J. An evaluation of clinical risk factors for estimating fracture risk in postmenopausal osteoporosis using an electronic medical record database. Osteoporos. Int. 2015, 26, 581–587. [Google Scholar] [CrossRef]
- Anagnostis, P.; Siolos, P.; Gkekas, N.K.; Kosmidou, N.; Artzouchaltzi, A.M.; Christou, K.; Goulis, D.G. Association between age at menopause and fracture risk: A systematic review and meta-analysis. Endocrine 2019, 63, 213–224. [Google Scholar] [CrossRef]
- Zhu, H.; Jiang, J.; Wang, Q.; Zong, J.; Zhang, L.; Ma, T.; Zhang, L. Associations between ERalpha/beta gene polymorphisms and osteoporosis susceptibility and bone mineral density in postmenopausal women: A systematic review and meta-analysis. BMC Endocr. Disord. 2018, 18, 11. [Google Scholar] [CrossRef]
- Jimenez-Mola, S.; Calvo-Lobo, C.; Idoate-Gil, J.; Seco-Calvo, J. Functionality, comorbidity, complication surgery of hip fracture in older adults by age distribution. Rev. Assoc. Med. Bras. 2018, 64, 420–427. [Google Scholar] [CrossRef]
- Briot, K. Fracture Liaison Services. Curr. Opin. Rheumatol. 2017, 29, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Mugnier, B.; Daumas, A.; Couderc, A.L.; Mizzi, B.; Gonzalez, T.; Amrani, A.; Villani, P. Clinical effectiveness of osteoporosis treatment in older patients: A fracture liaison service-based prospective study. J. Women Aging 2019, 31, 553–565. [Google Scholar] [CrossRef] [PubMed]
- Brozek, W.; Reichardt, B.; Zwerina, J.; Dimai, H.P.; Klaushofer, K.; Zwettler, E. Antiresorptive therapy and risk of mortality and refracture in osteoporosis-related hip fracture: A nationwide study. Osteoporos. Int. 2016, 27, 387–396. [Google Scholar] [CrossRef]
- Davidson, E.; Seal, A.; Doyle, Z.; Fielding, K.; McGirr, J. Prevention of osteoporotic refractures in regional Australia. Aust. J. Rural Health 2017, 25, 362–368. [Google Scholar] [CrossRef]
- Lyu, H.; Jundi, B.; Xu, C.; Tedeschi, S.K.; Yoshida, K.; Zhao, S.; Solomon, D.H. Comparison of Denosumab and Bisphosphonates in Patients With Osteoporosis: A Meta-Analysis of Randomized Controlled Trials. J. Clin. Endocrinol. Metab. 2019, 104, 1753–1765. [Google Scholar] [CrossRef] [PubMed]
- Pispati, A.; Pandey, V.; Patel, R. Oral Bisphosphonate Induced Recurrent Osteonecrosis of Jaw with Atypical Femoral Fracture and Subsequent Mandible Fracture in the Same Patient: A Case Report. J. Orthop. Case Rep. 2018, 8, 85–88. [Google Scholar]
- Black, D.M.; Abrahamsen, B.; Bouxsein, M.L.; Einhorn, T.; Napoli, N. Atypical Femur Fractures—Review of epidemiology, relationship to bisphosphonates, prevention and clinical management. Endocr. Rev. 2019, 40, 333–368. [Google Scholar] [CrossRef]
- Knopp-Sihota, J.A.; Cummings, G.G.; Homik, J.; Voaklander, D. The association between serious upper gastrointestinal bleeding and incident bisphosphonate use: A population-based nested cohort study. BMC Geriatr. 2013, 13, 36. [Google Scholar] [CrossRef] [PubMed]
- Palacios, S.; Silverman, S.L.; de Villiers, T.J.; Levine, A.B.; Goemaere, S.; Brown, J.P.; Chines, A.A. A 7-year randomized, placebo-controlled trial assessing the long-term efficacy and safety of bazedoxifene in postmenopausal women with osteoporosis: Effects on bone density and fracture. Menopause 2015, 22, 806–813. [Google Scholar] [CrossRef]
- Weaver, C.M.; Alexander, D.D.; Boushey, C.J.; Dawson-Hughes, B.; Lappe, J.M.; LeBoff, M.S.; Wang, D.D. Calcium plus vitamin D supplementation and risk of fractures: An updated meta-analysis from the National Osteoporosis Foundation. Osteoporos. Int. 2016, 27, 367–376. [Google Scholar] [CrossRef]
- Peng, L.; Luo, Q.; Lu, H. Efficacy and safety of bazedoxifene in postmenopausal women with osteoporosis: A systematic review and meta-analysis. Medicine 2017, 96, e8659. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Sui, L.; Gai, P.; Li, G.; Qi, X.; Jiang, X. The efficacy and safety of vertebral fracture prevention therapies in post-menopausal osteoporosis treatment: Which therapies work best? a network meta-analysis. Bone Jt. Res. 2017, 6, 452–463. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.; Wen, F.; Yang, W.; Xie, J.Y.; Ding, L.L.; Mo, Y.X. Comparative efficacy and safety of pharmacological interventions for osteoporosis in postmenopausal women: A network meta-analysis (Chongqing, China). Menopause 2019, 26, 929–939. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.F.; Wang, Z.Q.; Liu, L.; Zhang, B.T.; Miao, Y.Y.; Yu, S.N. A network meta-analysis on the short-term efficacy and adverse events of different anti-osteoporosis drugs for the treatment of postmenopausal osteoporosis. J. Cell Biochem. 2018, 119, 4469–4481. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Kang, N.; Yang, J.C.; Su, Q.J.; Liu, Y.Z.; Guan, L.; Hai, Y. Drug efficacies on bone mineral density and fracture rate for the treatment of postmenopausal osteoporosis: A network meta-analysis. Eur. Rev. Med. Pharm. Sci. 2019, 23, 2640–2668. [Google Scholar]
- Yang, X.C.; Deng, Z.H.; Wen, T.; Luo, W.; Xiao, W.F.; Zhao, R.B.; Li, Y.S. Network Meta-Analysis of Pharmacological Agents for Osteoporosis Treatment and Fracture Prevention. Cell Physiol. Biochem. 2016, 40, 781–795. [Google Scholar] [CrossRef]
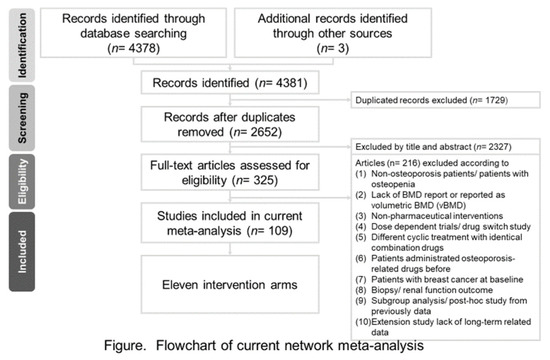
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Allon, R.; Levy, Y.; Lavi, I.; Kramer, A.; Barzilai, M.; Wollstein, R. How to Best Predict Fragility Fractures: An Update and Systematic Review. Isr. Med Assoc. J. IMAJ 2018, 20, 773–779. [Google Scholar]
- Gao, Y.N.; Wu, Y.C.; Lin, S.Y.; Chang, J.Z.; Tu, Y.K. Short-term efficacy of minimally invasive treatments for adult obstructive sleep apnea: A systematic review and network meta-analysis of randomized controlled trials. J. Med. Assoc. 2019, 118, 750–765. [Google Scholar] [CrossRef]
- Kendler, D.L.; Marin, F.; Zerbini, C.A.F.; Russo, L.A.; Greenspan, S.L.; Zikan, V.; Lopez-Romero, P. Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): A multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 2018, 391, 230–240. [Google Scholar] [CrossRef]
- Saag, K.G.; Petersen, J.; Brandi, M.L.; Karaplis, A.C.; Lorentzon, M.; Thomas, T.; Grauer, A. Romosozumab or Alendronate for Fracture Prevention in Women with Osteoporosis. N. Engl. J. Med. 2017, 377, 1417–1427. [Google Scholar] [CrossRef]
- Cummings, S.R.; San Martin, J.; McClung, M.R.; Siris, E.S.; Eastell, R.; Reid, I.R.; Trial, F. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N. Engl. J. Med. 2009, 361, 756–765. [Google Scholar] [CrossRef]
- Cosman, F.; Crittenden, D.B.; Adachi, J.D.; Binkley, N.; Czerwinski, E.; Ferrari, S.; Grauer, A. Romosozumab Treatment in Postmenopausal Women with Osteoporosis. N. Engl. J. Med. 2016, 375, 1532–1543. [Google Scholar] [CrossRef]
- Watts, N.B.; Grbic, J.T.; Binkley, N.; Papapoulos, S.; Butler, P.W.; Yin, X.; McClung, M. Invasive Oral Procedures and Events in Postmenopausal Women With Osteoporosis Treated With Denosumab for Up to 10 Years. J. Clin. Endocrinol. Metab. 2019, 104, 2443–2452. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, Q.; Yan, G.; Jin, X. Denosumab compared to bisphosphonates to treat postmenopausal osteoporosis: A meta-analysis. J. Orthop. Surg. Res. 2018, 13, 194. [Google Scholar] [CrossRef]
- Sanderson, J.; Martyn-St James, M.; Stevens, J.; Goka, E.; Wong, R.; Campbell, F.; Davis, S. Clinical effectiveness of bisphosphonates for the prevention of fragility fractures: A systematic review and network meta-analysis. Bone 2016, 89, 52–58. [Google Scholar] [CrossRef]
- Marjoribanks, J.; Farquhar, C.; Roberts, H.; Lethaby, A.; Lee, J. Long-term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database Syst. Rev. 2017, 1, CD004143. [Google Scholar] [CrossRef]
- Haguenauer, D.; Welch, V.; Shea, B.; Tugwell, P.; Wells, G. Fluoride for treating postmenopausal osteoporosis. Cochrane Database Syst. Rev. 2000, CD002825. [Google Scholar] [CrossRef]
- Gupta, M.; Gupta, N. Bisphosphonate Related Jaw Osteonecrosis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Kilic, E.; Doganay, O. Current management concepts for bisphosphonate-related osteonecrosis of the jaw: A review. Gen. Dent. 2018, 66, e1–e5. [Google Scholar]
- Nicolatou-Galitis, O.; Schiødt, M.; Mendes, R.A.; Ripamonti, C.; Hope, S.; Drudge-Coates, L.; Van den Wyngaert, T. Medication-related osteonecrosis of the jaw: Definition and best practice for prevention, diagnosis, and treatment. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 127, 117–135. [Google Scholar] [CrossRef]
- Gallacher, S.J.; Dixon, T. Impact of treatments for postmenopausal osteoporosis (bisphosphonates, parathyroid hormone, strontium ranelate, and denosumab) on bone quality: A systematic review. Calcif. Tissue Int. 2010, 87, 469–484. [Google Scholar] [CrossRef]
- Finkelstein, J.S.; Wyland, J.J.; Lee, H.; Neer, R.M. Effects of teriparatide, alendronate, or both in women with postmenopausal osteoporosis. J. Clin. Endocrinol. Metab. 2010, 95, 1838–1845. [Google Scholar] [CrossRef]
- Lou, S.; Lv, H.; Li, Z.; Zhang, L.; Tang, P. Combination therapy of anabolic agents and bisphosphonates on bone mineral density in patients with osteoporosis: A meta-analysis of randomised controlled trials. BMJ Open 2018, 8, e015187. [Google Scholar] [CrossRef]
- Lou, S.; Wang, L.; Wang, Y.; Jiang, Y.; Liu, J.; Wang, Y. Combination therapy of anabolic and nonbisphosphonates antiresorptive agents for the treatment of osteoporosis: A meta-analysis. Medicine 2017, 96, e9534. [Google Scholar] [CrossRef]
- Lou, S.; Lv, H.; Yin, P.; Li, Z.; Tang, P.; Wang, Y. Combination therapy with parathyroid hormone analogs and antiresorptive agents for osteoporosis: A systematic review and meta-analysis of randomized controlled trials. Osteoporos. Int. 2019, 30, 59–70. [Google Scholar] [CrossRef]